A Single Line as a Starting Point: Promoting Decision-Making in Therapy
 |
About the presenter: Lynne Shields is a professor in the communication disorder and deaf education department at Fontbonne University in St. Louis, Missouri, where she teaches courses in fluency disorders, language disorders, counseling and phonetics, and supervising in the university speech & language clinic. She is a board recognized specialist in fluency disorders. |
A single line as a starting point: Promoting decision-making in therapy
by Lynne Shields
from Missouri, USA
The use of self-rating scales in fluency therapy is not a new concept. Therapists across many disciplines use them in one form or another in treating clients. There are many excellent examples of scales available in publications or online. In this clinical nugget, I will focus on a very simple self-rating scale that can be modified to support active problem solving on the part of the client, as well as self-evaluation of progress toward therapy goals. I like using a paper-and-pencil task because it makes the process more concrete for both children and adults. It is something that can be looked at and talked about. Using a line, with or without numbers or lines marked on it, makes the notion of solutions as being on a continuum. Most choices are not all-or-nothing; rather, a client may elect to make a small change or a large change, depending on the perceived level of challenge.
To illustrate what I mean, I will use one case example to demonstrate a few ways to use the single line self-rating with clients. When the client is ready to do some problem solving about an issue, and this method seems appropriate to the task, I draw a straight line, horizontally or vertically, on a piece of paper as a framework. I try to keep the lines approximately the same length over time, so that the client and I can see changes over time. The end points are labeled according to the variable being rated or the hierarchy being considered. I prefer that the client generate the labels, but I generate the labels as needed.
1) Developing an understanding of steps in therapy
There are many great ways to help clients develop the notion of making small steps toward a goal in therapy. For example, Chmela and Reardon (2005) include a "Worry Ladder" among their self rating paper-and-pencil tasks. Situation hierarchies, one form of self-rating, are commonly used in therapy (see example by Diane Games below).
My case client, a 10-year-old boy named Chris, tells me that he finds it hard to talk to people other than family members, but that he would like to talk with more people in more places (his personal goal). I might begin with a line that will show his hierarchy of talking situations/partners, and have him label the two ends, filling in where various people or situations fall on the line.
The paper might now look something like Figure 1: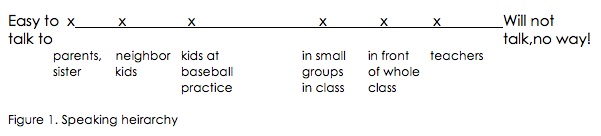
The two of us can talk about the situations or speaking partners on this line where he does/does not talk at the present time. Suppose Chris says that he will talk with kids at baseball practice, even if he is stuttering some, but he won't talk with kids in class, even in small groups, unless he is able to say what he wants using only one or two words, and definitely won't talk in front of the whole class or to teachers unless he absolutely cannot avoid it. Looking at the line, it appears that there is a gap between the baseball and small group categories, so I might ask if he ever talks to individual kids in his class, or, alternately, ask him to think about people or situations that he would place between those points. Chris can then add to the line where he sees fit; let's say he adds 'talking to Jack and Dave' midway between baseball and small groups on the line, and tells me that he is really pretty comfortable talking to both of them one-on-one at school. Once Chris is satisfied that, at least for the present, the hierarchy line is finished, we may talk about reasons why it is harder to talk in situations or to specific people on one end of the scale versus the other. Any ideas the child specifies can be written down on the paper for further discussion, and to help him come up with a plan of action.
2) Developing an action plan for outside practice
I am taking the term "action plan" from the work of cognitive behavioral psychologist Judith Beck (2011), who prefers that term to the more typical "homework" or "home assignment". She wisely points out that children aren't necessarily all that fond of homework, so any reference to activity outside of therapy as such may reduce the likelihood of a child (or adult) being interested in carrying it out.
Using the heirarchy line from above, I now want Chris to construct a plan that he will carry out between the current and following session. I may begin by saying, "so, you told me that you will talk to Jack and Dave in your class right now when it's just two of you together. And, that you will talk in your small group time if you only need to say just a few words. I wonder if there is a situation or person between those two points where you are willing to challenge yourself to talk this week." With help as needed, perhaps Chris decides that he would first like to talk to Barry, a boy in his class whom he likes, but to whom he rarely speaks. We can add 'Barry' to the line, and discuss how he plans to go about accomplishing this task. When will there be opportunities to talk with Barry, what might he say to him, how many times he wants to target for talking, and how he will keep track of talking times. This is then put in writing, preferably by having Chris write out his action plan for the week. It can be written on the same paper with the hierarchy he has constructed, so that this visual will go home with him. If Chris is a bit nervous about doing this, we can engage in some role play before the session ends. To further enhance the likelihood of success, I may ask him to rate how likely he is to carry out the action plan as we talk about it, using another line that might look like Figure 2:
If he places his mark close to the 'probably won't', that tells me we need to either revise the plan to a higher comfort zone, or do some more exploring of his concerns. When he rates himself closer to the "definitely will", both of us are probably more confident about Chris actually doing the task he set for himself. Alternately, this can be done verbally. He can give his answer in percent ("I'm 70% likely to do it") or choose from three or four choice points (not very-a little -moderately-very likely). If I have Chris rate himself verbally, I then write his answer down on the action plan.
3) Assessing progress in therapy
Between session progress:
During the next session, I will be sure to ask Chris about how his action plan worked out. If he tells me that he talked to Barry three times throughout the week, we engage in discussion about whether that met the goal he set in his plan. If so, I comment on his ability to set a goal, make a plan and carry it out. I might draw another line (as in Figure 3), and ask Chris to rate how easy he thought it was to talk to Barry: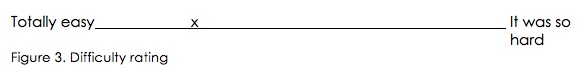
Perhaps he rated himself as above. A follow up discussion for this might include talking about how it was a little hard to do, but he did it anyway, why it takes effort to try new things, what he might choose to do so that the mark will move toward the 'easier' end of the line over the next week or two. Either Chris or I record his thoughts below the line. Talking it over with the help of the visual rating can facilitate the process of developing his action plan for the following week. Chris may decide that he thinks it will be easier if he stays on the same plan because it will feel even better with more practice. I want to be sure to tell him, "that sounds like a really good reason to stick with this plan for another week", affirming his ability to think about the issue and make a decision. If, on the other hand, he says that he wants to choose to talk twice every school day to Barry, or perhaps add another child, I affirm this decision in a similar way. Having the child make informed decisions is more important to me than the specifics of any particular plan. Helping Chris look at and evaluate the outcome of his action plan facilitates his ability to independently figure out how he can make changes in his life.
When a client comes in and had not met the action plan, this is a great opportunity to review the ratings and action plan in view of revising both. For example, if Chris reports that he could not work up the nerve to talk to Barry, we may talk about what made it harder than he anticipated, or in what ways the action plan was perhaps not really what he needed right now. Going back to his speaking hierarchy (Fig. 1), I ask Chris to take a look at the points he marked on the line and decide if the 'distance' between Jack/Dave and Barry is bigger than he had anticipated. Or, if he placed a mark much closer to "it was so hard" on Figure 3, I might draw an arrow pointing to a position a small distance from his mark toward "totally easy" (see Fig. 4). I could ask Chris what he might do to would move his self-rating just that little bit closer to "it was totally easy". Asking this simple question with a very short distance toward positive change noted on the line may be enough to help Chris come up with a revised action plan that is at a higher comfort level and more do-able.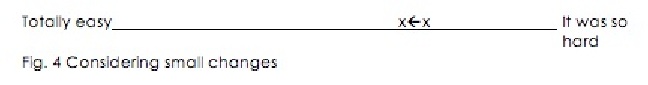
Longer term progress:
Another important part of assessing progress in therapy involves having the client look back at his progress over a longer period of time. For the above goal of talking to more people or in more situations, Chris and I can revisit the hierarchy he developed after several months of therapy. He may find that when he marks people and talking situations on the line after a period of time, more items are now placed closer to the "easy" end of the line, compared to his first rating, or that his end points have now shifted; the right hand label is now "will talk sometimes". This gives him visual evidence that he has made measurable progress. Both children and adults benefit from seeing clear evidence of change in therapy. Seeing these changes on paper is likely to enhance the feeling of success and increase motivation for further change.
These are just a few examples of ways to use a line self-rating scale in therapy. The needs and wishes of the client dictate when and how this type of self-rating can be of benefit. I hope that those of you reading this paper will share other ideas on the threaded discussion. I look forward to hearing from you.
References:
Beck, J. S. (2011). Cognitive behavior therapy: Basics and beyond. New York: The Guilford Press.
Chmela, K. A., & Reardon, N. (2005). The school-age child who stutters: Working effectively with attitudes and emotions. Memphis, TN: Stuttering Foundation.
Games, D. (accessed 7/9/2012). Situational anxiety hierarchy. Available at: http://www.fluencyfriday.org/Situational%20Anxiety%20Hierarchy.pdf.
SUBMITTED: July 13, 2012

