Clinician's Guide to the Stuttering Clinic
Gary J. Rentschler, Ph.D.
This manual was constructed to support you in the Stuttering Clinic. While it likely won't answer all of your questions, please consult this material as a "first line of defense" as you learn to work with clients who stutter.
Table of Contents
PAGE 1
Basic Skills for Stuttering Therapy
This segment contains information about the basics of therapy for stuttering to orient you to the Stuttering Clinic and provide you with a resource for basic information regarding clinical instruction.
It is hoped that in working together this semester your clinical skills and experience will grow and that your client will benefit from your therapy. Over the course of the semester I will expect you to demonstrate growth in terms of your ability to work independently and problem-solve on your own. But at the beginning, I strongly encourage you to ask a lot of questions and consult this information packet regularly.
What to Expect
Some comments from the experiences of other students are shared below. Their experiences may help to shape your expectations of the learning process.
"Counseling is a major part of stuttering therapy. At first, I felt that this 'talk therapy' wasn't really speech therapy and that I wasn't really working on the client's stuttering. I came to find out that this 'cognitive-emotive' therapy plays a role equal in importance to the speech goals. In the beginning, I felt I was 'just talking' to the client. But you, and the client, gain valuable insights into the way the client experiences stuttering. We worked to 'reframe' the way he thought about his disfluencies, which proved to be most helpful for him."
"It took me a while to pick up on the subtleties of my client's stuttering, particularly because the severity of his overt symptoms was so mild. He tried to hide his stuttering too; at first I didn't know that. He also avoided words he was afraid he'd stutter on and used other words instead. It took me a while to catch on to that, too. I saw other clients who stuttered only once or twice per session. Each person who stutters does so in a different way. If you are expecting each disfluency to be a 'significant event', that may be your first surprise in working with this disorder."
"My client had difficulty figuring out how he felt about his stuttering because he was in such strong denial. He didn't seem to be objectively aware of his overt symptoms. This was really amazing to me in light of the severity of his stuttering."
"When I started out, I was real reluctant to interrupt my client in the middle his stuttering to give him instructions, reminders and cues. I learned later that this was part of my job as his clinician. He later said that he was appreciative of my guidance at those difficult times and relieved to be given permission to stop struggling and start over. I would have never guessed that that was what he was feeling!"
WRITING LESSON PLANS
A lesson plan is the basic means of organizing, planning and communicating a treatment session. You will also find your lesson plans helpful in documenting your work and the client's progress each session. Each client has a number of goals established to guide the course of his therapy. A lesson plan is a series of behavioral objectives that systematically address the goals for your client, based on his level of performance. The lesson plan details the activities and materials to be used in the session, which helps me to assess what you are doing and how you are thinking.
Planning begins with the goals established for the client. From these goals, behavioral objectives are written, designed in an instructional format and supported by a pedagogical rationale that systematically work the client through exercises designed to promote his or her development of desired skills. Initially, baseline data is collected to establish the client's current level of functioning. From the baseline, performance criteria are
PAGE 2
established, that will challenge the client and enable him to learn and progress. Data based upon the client's actual performance level is reported in the progress notes. The lesson plan is merely a tool used to design the session. Lesson plans are not required to be filed in the patient's file, but progress notes are.
Basic Components of the Lesson Plan
Lesson plans are reviewed weekly. They need to be submitted electronically, no later than 48 hours before the session.
The Goals are generally established for the semester; they may be revised during the course of the semester should new information be revealed, or significant progress be achieved. A client usually has about three general goals they are working toward.
The Behavioral Objective describes specifically what is expected of the client in a particular activity. Behavioral objectives often change from week to week, based upon the client's performance level.
Briefly describe the Activity you wish the client to engage in for each behavioral objective. Provide enough information so the reader can get a feel of what you plan to do.
List the Materials you intend to use in each activity.
Your Clinical Instructor may wish to make Comments or suggestions as part of the lesson plan; there is a section on the form for them to do so. The lesson plan may be returned before the session or discussed with you. It is recommended that you save a copy of your lesson plan on a memory stick; it will facilitate your work and save you time throughout the semester. Remember to use only the client's initials when sending information electronically.
Developing a lesson plan is a basic clinical skill. The fundamental units of the lesson plan are the Goal and Behavioral Objective. The Goal represents the bigger picture, or a major thrust of therapy. The Behavioral Objective designates one step toward that goal. For example, a Goal might be to increase a patient's objective knowledge of his stuttering. A step toward that goal might be to have the client identify each disfluency and describe the type (repetition, prolongation, block) that he evidenced.
WRITING BEHAVIORAL OBJECTIVES
The following therapy objectives are offered as models for clinicians. Many, working for the first time with clients who stutter, find it difficult to write therapy objectives to incorporate a criterion, "do" statement, and condition in behavioral terms. These samples are presented in a general format in the primary areas of therapy and may need to be adapted to meet the unique needs of individual clients. The specific goals, techniques, and criterion measures will vary based upon the needs and level of each patient. A goal and corresponding sample behavioral objective (BO) follows:
- (1) SPEECH AWARENESS
- Goal: Increase awareness of stuttering
- BO: While reading a passage aloud, the client will raise his hand to identify 90% of his disfluencies.
- (2) SPEECH DESCRIPTION
- Goal: Increase awareness of stuttering
- BO: When asked, the client will accurately describe the type and identify the place of his disfluencies eight of ten times.
PAGE 3
- (3) SPEECH MODIFICATION
- Goal: Stuttering modification target use in conversation
- BO: The client will implement the pull-out technique in three of four disfluencies.
- (4) SPEECH PREPARATION
- Goal: Fluency shaping target use in reading.
- BO: The client will use gentle onset prior to initiating words he anticipates he will stutter on 85% of the time while reading a passage.
- (5) EMOTIONAL AWARENESS
- Goal: Increase awareness of anxiety
- BO: The client will identify three physical indicators of his anxiety immediately prior to introducing himself to a group of novel people.
- (6) EMOTIONAL EXPLORATION
- Goal: Increase understanding of emotional stressors
- BO: The client will recount in detail three instances from childhood that precipitated negative emotional reactions to stuttering.
- (7) EMOTIONAL MODIFICATION
- Goal: Managing emotional reactions
- BO: On three occasions prior to speaking to a group of people, the client will pause, take a deep breath, exhale slowly, and monitor the release of muscular tension in one part of his body.
- (8) EMOTIONAL/SPEECH MODIFICATION
- Goal: Stuttering modification target use in conversation
- BO: Given a cue, the client will continue a disfluency for at least 15 seconds duration on eight of ten instances of stuttering.
- (9) EMOTIONAL/SPEECH MODIFICATION
- Goal: Awareness of anxiety
- BO: When asked, the client will identify three fears before speaking, the effect that fear habitually has on his muscular tension, and how he will compensate for the impact of its habit strength, three times during the group session.
- (10) EMOTIONAL/SPEECH MODIFICATION
- Goal: Identification of stuttering
- BO: The client will describe five components of his stuttering pattern and identify the speech strategy to accommodate the impact of its habit strength.
- (11) EMOTIONAL UNDERSTANDING
- Goal: Demonstrating knowledge of stuttering
- BO: The client will formulate one plausible reason for his stuttering and explain it to someone outside the Clinic.
- (12) EMOTIONAL MODIFICATION
- Goal: Acknowledging stuttering
- BO: The client will explain that he stutters occasionally to his listener after his first disfluency speaking on the telephone.
PAGE 4
- (13) EMOTIONAL MODIFICATION
- Goal: Increasing objectivity toward stuttering
- BO: After speaking to a group of people, the client will give a balanced critique of his speaking performance to include his (a) his management of his stuttering, (b) overall fluency, (c) ability to implement slow rate, and (d) the success in communicating the content of his message.
- (14) EMOTIONAL UNDERSTANDING
- Goal: Understanding emotions of stuttering
- BO: After being disfluent, the client will identify three components of the emotions he experienced during his disfluent moments.
- (15) EMOTIONAL MODIFICATION
- Goal: Modifying emotional reactions to stuttering
- BO: On two occasions the client will intervene in his pre-speech self-talk, interjecting rationally-based comments just prior to initiating speech.
- (16) SPEECH MODIFICATION
- Goal: Increase fluency shaping target use.
- BO: Without cueing, the client will initiate speech using gentle onsets in four consecutive utterances.
STRUCTURING INDIVIDUAL THERAPY SESSIONS
The following format guide in structuring individual therapy sessions is offered as a starting point for new fluency clinicians. While this format is designed specifically for stuttering therapy, it is based on principles that apply to therapy for other disorders as well.
Set the tone for the session by getting started right away. Your interaction begins in the waiting room; get your "chit chatting" done on the walk to the treatment room. As soon as you are seated in the therapy room, start off by reviewing homework assignments given at the last session. After that you may find the following protocol to be useful in designing your session.
Overview: Review the outline of what you want to do and accomplish in the session with the client. This will orient him to what will happen and his role in the session. Your organization and preparedness will be noted by the client.
Warm Up Activity: (5-10 minutes) A period of speech target practice in which the clinician provides intensive cueing and feedback. This gets the client "on track" right away, enabling you to demonstrate his proficiency level; it also sets a tone that "we're here to work"! Continue until the client achieves the expected level of proficiency.
Activity Two: Work Activity (5-10 minutes) During this speech activity, don't give any cueing or feedback; see how the client does on his own. You'll likely observe some things about the client's performance that you can convey after their performance. If the client does poorly, give them the necessary feedback to make the desired improvements.
Activity Three: Work Activity (15-20 minutes) This may be a speech or "feelings" activity. If it's a speech activity, make the first part "too hard" for the client, so he struggles; then change one parameter so it will boost their success rate significantly.
If you choose a "feelings" activity, try to conclude on a positive note by pointing out a lesson learned or a new insight into their stuttering that resulted from the discussion.
PAGE 5
Back Up Activity: (10 minutes) Despite your best planning, some activities just "don't work". Have another activity prepared; if you don't use it, you'll have it for another time.
Homework Assignment: It's vitally important that your client have something to work on each day to expedite his progress and carryover. Have a specific task for your client to do at least every day. Work out a specific time or situation that the client will accomplish the assignment. Try to problem-solve any obstacles with your client, including them in the process.
Wrap Up: At the very end, summarize what was accomplished in the session today, providing complements and constructive criticism. Talk about the next steps in therapy and what you hope to accomplish during the next session. This is an important part of your clinical teaching.
Lesson Plans. A written lesson plan is submitted each week. If your client comes to therapy more than once per week, only one lesson plan is necessary for each week.
STRUCTURING GROUP THERAPY SESSIONS
Group therapy is a workplace to practice speech targets and to build bonds with others who stutter. For most clients, speaking before a group of people is significantly more difficult than practicing in the relative comfort of individual therapy sessions. Group is therefore, a situation that most clients find more challenging. Group therapy is also used as a forum for learning and sharing stuttering experiences. Many clients have neither talked about their stuttering much nor hear others speak about their experiences. The group environment then offers a dual purpose in the therapeutic process.
Group often follows a standard format each week, although you are welcome to discuss how the protocol can be altered to accomplish your goals. Clinicians take turns each week being group leader. Most sessions devote time to practice speech targets and time for sharing. The following is the general format for group:
Welcome. The group leader calls the session to order and offers a topic for everyone to give a brief extemporaneous response. The leader begins the activity by standing, introducing him/herself and responding to the topic. Each person takes a turn by standing, introducing him or herself and speaking.
Check-In: The group leader asks each client about his/her speech over the past week. Next, each client is asked which speech targets they will be using during group and the particular goals they have set for themselves.
Activity One: The group leader instructs participants for the activity. Often a sharing activity is first. Occasionally, clinicians attending group participate too. The leader may modify their participation as deemed appropriate; the objective is to maximize client participation time, yet still include comments from all group members. At the end of the activity, the leader summarizes the discussion and highlights key points that surfaced from the activity.
Activity Two: A second activity is introduced; usually directed at speech target practice. Student clinician participation is usually limited, giving clients more opportunity to contribute. Again, at the conclusion of the activity, the group leader summarizes the activity and each client's performance.
It is often wise to plan a third activity as a back-up. Some activities do not take as much time as planned or might not be meeting intended objectives. They can be stopped and the back-up activity used in their place.
Wrap-Up: At the very end, the group leader critiques each client's performance during group and the success they demonstrated incorporating their goals and target use. A client's self-evaluation or client-to-client assessment is sometimes a part of the critique.
PAGE 6
Tips for Leading Group Sessions
Lesson Plans: A written lesson plan is not required for group; plans for group will be discussed in a weekly supervisory conference prior to the clinician leading group. It is anticipated that the clinician will be prepared to discuss the plan for group therapy. Ways of increasing client participation or other slight modifications are often suggested by the Clinical Instructor.
Progress Notes: Each clinician should monitor the performance of their client in group. It is their responsibility to include this information in the progress notes. It is important to describe the activities as well as the client's performance in the notes. Make progress notes clear and easy to follow. If a client has individual and group therapy on the same day, one progress note can be used for both sessions.
CUEING AND GIVING FEEDBACK
Giving instructions, feedback and cueing are critical teaching tools in any therapeutic interaction. These are the primary vehicles used to shape behavior and should be used liberally through treatment sessions.
Most beginning clinicians are reluctant to interrupt the client when he is speaking; the usual concern is that it's impolite. This is business and it is now part of your job as the clinician to guide the client. Most clients are relieved to be given permission to stop in the midst of their stuttering, given some instruction, and begin again. It helps the client improve more rapidly.
Be "tough" on your client; require responses that are really good. Use the criteria you have established to successfully accomplish each task. Your therapy will be better and your client will progress faster as a result. "Shaping" your client's responses by providing consistent feedback is a vital part of their learning process. If the client isn't demonstrating a proper response, correcting them (guiding them) is an important channel for change. Be stringent, be fair, be consistent... your client will respect you for it.
As you become more familiar with your client, you will develop a sense of when to push harder and when to back off with your feedback. Ideally, you'll go up to the "line" but won't cross it.
After each activity, critique your client's performance. Balance your evaluation by providing positive and constructive criticisms. A pattern of providing positive, constructive, and lastly positive feedback can put an upbeat spin on your critique. While it's always nice to hear complements, real growth comes out of constructive suggestions. Don't fall into the habit of only providing complements; your client will see right through that and you'll lose credibility.
FIRST SESSION ADVICE
Stuttering is an exceedingly difficult and often frustrating problem to treat as progress is usually slow, clients resist changing behaviors, and stuttering itself is so variable. Many clinicians are somewhat apprehensive about working with adults and adolescents who stutter; they often fear they will make the stuttering worse or are unsure of what to do. A few suggestions are offered to assist you in your first therapeutic encounters.
Focus on Speech Therapy First. The point has been made that stuttering therapy deals with both speech behaviors and the psychodynamic aspects that result from stuttering. Start with the speech behaviors. Having a reliable speech technique is invaluable and the backbone of effective therapy. Clients are unlikely to share much of their feelings and emotions about stuttering with any new clinician; it takes time to get to know someone and trust them.
PAGE 7
Have a Strong Rationale for What You Do. Know what you are doing, and why, in each component of your therapy session. The best therapy is usually "client-centered"; if you thoroughly understand your objective, making the adjustments and alterations based upon your client's individual needs will be much easier.
Keep Perspective. Remember above all you are working with a person, not just a problem. The problem has significance in the person's life and that's the important part.
First Session Accomplishments. By the end of the first session you should:
- Be able to describe the client's stuttering behaviors
- Set a "down-to-business" (rather than "casual-social" conversation) tone for your session right from the start
- Learn what your client wants to accomplish in their therapy
- Be clear that the client is responsible for making the changes, that you are the guide or mentor right from the start, by the language that you use your orientation toward problem-solving
- Give daily homework assignments that require some form of verification
Don't:
- Focus on counting disfluencies
- Waste time - therapy time is valuable and expensive; most people spend more time watching television commercials each week than spend with you in therapy — you need to make an impact in each session
- Concentrate on your own anxieties, it just heightens them; the therapy isn't about you anyway. If you are anxious, it just shows that you want to do a good job. If you didn't care, you wouldn't be anxious.
- Use more than your "share" of the speaking time; the client should do more talking than you do
The initial meeting with any client is usually the most difficult because the "unknowns" are much greater than the "knowns". First impressions are important, but it takes time for a therapeutic relationship to develop. Be organized, set your agenda, be direct and speak authoritatively, and enjoy the new clinical challenge.
WRITING PROGRESS NOTES
A progress note is written for each visit, even if the client cancels. It is a legal document that serves as a record of each session. It is important to describe the activities as well as the client's performance in the notes. The SOAP format is used for progress notes: it includes the following components:
- Status A statement that describes factors that may affect the client's performance on the day of the session. For example, if he came late or was tired from his day at school, or if he was accompanied to the clinic by a parent on that day.
- Objective This section reports the client's performance level in each activity administered during the session. It is usually very cut and dry, just reporting factual data. Note that it is structured exactly like the behavioral objectives from the lesson plan, only the actual performance level is reported instead of the projected performance level on the lesson plan.
- Assessment In this section you interpret the client's performance that day, comparing it perhaps to previous sessions, or highlighting significant advances, or reporting potential obstacles to progress revealed in the session.
- Planning As a result of the client's performance and in light of the long- and short-term goals, the clinician makes statements about what she will do in upcoming sessions as a result of today's session.
Another way of looking at SOAP notes might be to say, Here's the situation when the client arrived today; this is how he performed; this is what I believe it means (how I interrupt it); and, as a result, here is what I intend to do the next session.
PAGE 8
Progress notes are a legal requirement under PA Code (law) and a fundamental component of competent clinical practice. It is the official record of your work. A progress note is required for each session. As the saying goes, If it's not documented, you didn't do it. You will learn in the Seminar Class that documentation is a means for speech-language pathologists to protect themselves.
While the progress note is used primarily by the clinician, it may also be read by others. For example, clients also have a legal right to request a copy of the notes; third-party payers (like insurance companies) may require progress notes to continue funding therapy; and in the event that another clinician may need to cover a session for you, they will want to read notes to prepare for the session. Thus progress notes should be written for a variety of readers.
THE SUPERVISORY PROCESS
Clinical Supervision is a mentoring process. The overall objective is to build independence in the student clinician. It is usually up to the clinician to demonstrate their independence; part of the role of Clinical Instructor is to evaluate your skills and growth along this parameter. One way I can do this is by providing resources to you, such as this manual. Our weekly conference meetings, in which we discuss specific aspects of clients and your therapy, is another. Throughout the process it is incumbent upon you to ask questions. Asking questions indicates to me that you are aware that you don't have all the information that you need; this illustrates that you are at a higher level than not being aware that you don't know an important piece of information. A still higher level would be being cognizant that you don't know something and being able to generate possible answers.
Taking risks is an important part of learning. Sometimes risks result in failures. But taking risks and failing enables you to learned more quickly; if you only attempt things you are sure will succeed, you are spending too much time in your comfort zone. Learning also comes from successes, but my role as mentor is to push you out of your comfort zone, minimize the impact of your failures, and generate a lesson from the experience.
A Starting Point. We begin by meeting before your first session with a client to discuss his communication needs, review the therapeutic process, and plan for the first session. This doesn't always happen in one meeting, so additional time may be required. By the end of the meeting you should be prepared for the first session.
Observation. I will observe each of your therapy sessions. ASHA requires that you be observed at least 25% of the time; in most instances I observe much more than that. From my observation, I complete an Observation Report with notes and comments. You will find the Observation Report in your mailbox shortly after your session. Be sure to bring it to our weekly meeting to discuss if you have questions. If you have more immediate questions or concerns, please feel free to stop by and arrange a time for us to meet. I often come into the therapy room to talk with the client, try a therapy technique, or demonstrate something for you. Coming into your session is not an indication that something has gone wrong! I enjoy working with the patients too.
Weekly Group Conferences. We will establish a weekly meeting time to discuss the clients, your performance in clinic, and any other issues pertinent to therapy. The standard weekly meeting time is usually established at the beginning of the semester. Please remember to bring the Observation Report to this meeting.
Lesson Plans. After the first session, you will need to prepare a weekly lesson plan. The lesson plan is due 48 hours before the session. We will review your plan at the weekly conference. Only one lesson plan is required for the week, even if the client comes multiple times during the week. Be sure to include goals and behavioral objectives for group therapy as well (if appropriate). Submit your lesson plan on the appropriate form, attaching it to an email to me. Be sure to use the client's initials, not their name on the lesson plan. Lesson plans are not filed in the patient's chart. It is wise to save an electronic copy of each lesson plan on a memory stick so it is easier to revise them and generate a new one for the next week.
PAGE 9
Progress Notes. Progress notes are due 48 hours after each therapy session. It is easiest to complete progress notes immediately after your session if your schedule permits. Using the appropriate form, submit your completed progress note to me by attaching it to an e-mail. For security, do not use the client's name. If the note requires revisions, I will send it back to you with an explanation. If it is fine as is, or only needs minor editing, I will take care of that, print it out, sign it, and place it in your mailbox for your signature. You will then turn the note in to the Clinic Office to be filed in the patient's chart.
Evaluation. At mid-semester, I will complete a Student Practicum Evaluation form and we will review it together. While you will be receiving feedback each week, this is the time when you are formally evaluated. We will discuss your achievements and plan to work on other areas to continue your growth. The mid-semester grade counts toward 40% of your total grade.
The week following the conclusion of clinic, we will again meet and review your Evaluation. Your semester grade will be determined at this time., with 60% stemming from the end of semester evaluation.
General. It is hoped that the supervisory process will be an open exchange. Don't be hesitant to admit you don't know something! It will be apparent sooner or later anyway. Letting me know that you don't know something enables me to help you learn more rapidly — and that's why we're both here!
OVERT SYMPTOMS OF STUTTERING
There are several features of stuttered speech that are visible to the observer. The overt signs of stuttering constitute the most obvious and readily identifiable symptoms of the disorder. They are what people think of when they think of stuttering. Overt symptoms include the following speaking behaviors:
Blocks. Blocks are stoppages of the flow of exhaled air during the process of speaking. They usually occur at the level of the vocal folds (laryngeal block) or in the oral cavity when one of the articulators (usually the tongue or lips) serve to occlude the passage of air. Many patients struggle, using extra effort to try to overpower and push through their blockages. Consequently, the desired sound is not being produced. The only sound that may be heard is that of the struggle trying to force through the block.
This results in the blocks appearing more severe. The patient appears "stuck" with no air being exhaled during the block. Blocks usually occur at the beginning of sentences, beginning of words, or on the stressed syllable of a word; almost never at the end of a word.
Repetitions. A repetition is when a sound or syllable is repeated, generally two or more times — sometimes many more times. Some repetitions are very rapid; almost faster than one could repeat the sound or syllable volitionally. Some who stutter stop themselves once the repetitions start; others will continue on as if to try to outlast the disfluency.
Prolongations. A prolongation is the continuation of a sound well beyond its normal duration in speech. It appears as though the speaker is "stuck" on the sound, unable to transition to the next sound in the utterance. Prolongations are similar to blocks, except with a prolongation, the desired sound is being produced; the speaker's difficulty is moving to the next sound in the sequence.
Tremors. Muscular struggle and excessive tension, particularly in the jaw, can result in rapid oscillations of the jaw, known as tremors. Tremors are rare relative to other overt symptoms of stuttering. The rate of oscillations is more rapid than is possible to replicate volitionally.
PAGE 10
The overt features of stuttering are one of three categories of stuttering characteristics. While the overt features are often very pronounced, in many patients, they are very subtle and can only be noticed if the patient's speech is very closely scrutinized. Additionally, many who stutter intentionally try to mask or avoid displaying these noticeable signs of their stuttering. Consequently, the clinician must look and listen extremely carefully to detect these overt symptoms.
COVERT FEATURES OF STUTTERING
The vast majority of clients who stutter have a lot going on "under the surface". These covert features include behaviors to avoid stuttering and the feelings and beliefs about their stuttering. The feelings and beliefs often drive many of the behaviors associated with the stuttering pattern. Therefore it is vitally important to understand how the person who stutters thinks about their stuttering in order to determine where the behaviors originate.
Some who stutter seek to hide their stuttering by a variety of means. Generally, the overt severity of stuttering among covert stutterers appears to be very mild. However this does not mean that the handicapping effects of their problem are any less than those stuttering overtly. One common trick is to substitute words, using a word you can say for one you fear you will stutter on. Word substitutions often complicate the attempt to formulate the message that was intended. Sometimes branching to other (substitute) words clouds the message and can sound confusing to the listener. Try saying a few sentences and changing every third word that you want to say. Notice how much mental effort is spent in word selection —- better open up the thesaurus! And in the process note how your sentences sort of weave in, out and around your intended thought stream. Most people find this mentally exhausting; but apparently better than stuttering!
Others avoid stuttering by not talking or talking very little; they are often thought of as being shy. They often structure their world around their stuttering..... ordering what they can say in a restaurant, not answering questions in class when they know the answer, or driving over to someone's house instead of calling them on the phone.
The real handicap of stuttering is how the person feels about him/herself, as a person and as a communicator. All people who stutter let their stuttering affect the decisions they make; for example, what they order at a restaurant something they can say or what they actually want. Some who stutter have someone else order for them. So imagine how you would feel having dinner with your parents and a few friends and needing to have your mother order for you! Still others just don't go the restaurants at all. In getting to know your client, you will learn how stuttering impacts his/her life.
STUTTERING CONCEPTS AND TERMINOLOGY
Over the years, a multitude of terms has been used to describe and define the techniques or approaches in fluency therapy. In many instances, it is exceedingly difficult to trace the etiology of the terms to their originators. The list below, therefore, does not attempt to identify the etymology of the terms, but merely presents a compilation of terms often used in regard to fluency therapy.
ADAPTATION - Reading the same passage multiple times, the number of disfluencies decreases in each successive reading. (Of marginal clinical value; may be helpful in desensitization)
AIRFLOW - Beginning the process of speaking by releasing more air than usual (exhalation) just prior to gently adducting the vocal folds to initiate phonation. (Reduces laryngeal blocks)
ALCOHOL - Many people who stutter report alcohol consumption diminishes anxiety and they become more fluent. Others find it diminishes their control of speaking and they become more disfluent.
BIBLIOTHERAPY - Providing written materials to educate and inform a patients about the nature and treatment of their stuttering problem. (Enhances patient's understanding and establishes a working vocabulary)
PAGE 11
BOUNCING - "Breaking up" the tension of a block by changing it to a controlled repetition. (Modifies laryngeal and oral blocks)
CANCELLATION - A beginning stage in modifying a stuttering block by first finishing the stuttered word, pausing one or two seconds, then repeating the word using very slow motion and smooth, gradual transition from sound to sound. (Primary step in modifying/changing stuttering pattern)
CHANTING - Speaking in a "chant" or singing manner that utilizes continuous phonation with reduced rate and inflection. (Enhances the feeling of speech as continuous movement; minimizes blocks, repetitions and tremor)
CONTINUOUS, FORWARD BALLISTIC MOVEMENT - Speaking at a reduced rate, emphasizing only articulatory movement to the next successive sound in the sequence — no backing up or repeating (Reduces avoidances and disrupts stuttering pattern)
CONTINUOUS VOICING/PHONATION - Maintaining the feature of voicing throughout the articulation of an entire utterance. (Reduces blocks occurring after initiation of utterance)
DELAYED AUDITORY FEEDBACK (DAF) - Changing the patient's audition of their own speech by altering (increasing) the time between production and self-audition. (Slows rate and enhances oral proprioceptive feedback)
DELAYED RESPONSE - Waiting a few seconds before responding to your communicative partner. (To slow overall rate of speaking and exert volitional control of speaking)
DRUGS (PRESCRIPTION) - Use of a drug that reduces overall anxiety. Milder stutterers often report some success; more severe stutterers generally find the drug insufficient, as fears/anxieties may be sudden and too intense at the moment when speech is attempted. Experimentation with other drugs (such as Clomipramine and Desipramine) is currently ongoing; some patients report fewer disfluencies with Clomipramine.
EASY or GENTLE (VOICE) ONSET - Initiating phonation by emphasizing gentle contact of the vocal folds; secondarily slows rate at onset of utterance and reduces tension. (Reduces laryngeal blocks)
EASY SPEECH - A combination of techniques which serves to enhance fluency by using less effort to speak. The term is most often used with children.
EASY STUTTERING - Modification of stuttering that reduces struggle behavior and affords a feeling of better controlled speaking. (Changes stuttering pattern and reduces severity of blocks)
ERA-SM - A technique which begins by combining slow rate, slight syllable stretch, light articulatory contact and gentle onset at initiation of an utterance, then allows rate to increase while emphasizing ballast movement.
FLOODING - Purposefully stuttering on each word uttered. (Reduces laryngeal and oral tension; diminishes fear of stuttering - desensitizes)
FREEZING - Continuation of a block for several seconds until it is under voluntary control. (Builds feeling of controlling stuttering blocks, reduces tension in the block)
GILCU - Gradual Increase in Length and Complexity of Utterance. A learning process in which fluency is positively reinforced through a series of progressively longer and linguistically and/or articulatorilly more complex material.
PAGE 12
GOING TO THE WORD - Patient is instructed not to avoid, postpone or circumlocute uttering a particular feared word, but rather to begin articulating it directly, generally using a control technique. (Diminishes fears and avoidances)
HYPNOSIS - Using post-hypnotic suggestion to reduce anxiety in feared speaking situations. Most report only temporary results, if any.
IMAGING - A psychological technique of projecting yourself into a difficult speaking situation and visualizing yourself being successful.
LIGHT (ARTICULATORY) CONTACT - Articulation using minimal muscular effort in making contact at point(s) of articulation. (Diminishes oral blocks and repetitions)
LOW PITCH VOICE - Beginning an utterance using a low-pitched voice. (Requires patient to be relaxed in speaking situation to reduce tension on vocal folds)
METRONOME EFFECT - Speaking to the imposed rhythm of a continuously swinging arm, finger or metronome. (Of limited clinical value; may demonstrate that a person can exert control over his or her stuttering)
PACKAGING - The concept of focusing on one technique that brings other techniques into play. (For patients who have been in therapy and experienced success with several techniques)
PREPARATORY SET - "Scanning" for potentially difficult words, planning ahead to utilize a speech target prior to initiating the attempt to speak the word. (A more advanced strategy to minimize stuttering)
PROLONGATION - A means of modifying a stuttering block by stretching it out just after the block has begun. (Useful to teach control of oral and laryngeal stuttering)
PULL-OUT - After a block has begun, the patient stretches the stuttered sound until he has gained control of it (Helpful to learn to control stuttering blocks)
RELAXATION - Numerous techniques that serve to lessen muscle tension and promote greater relaxation while speaking. May have positive benefits in preparing to give a speech or presentation, if individual has the time to access a "relaxed state" prior to speaking. Generally insufficient in situations that don't allow for preparation. (Builds awareness of tension and provides a means to dissipate it, but usually requires too much time)
SCANNING - Looking ahead to words about to be spoken for potential difficulty to implement speaking techniques avoiding having a stuttering block. (Builds awareness and control and forms basis upon which to build confidence)
SHADOWING OR PARROTING - Stutterer and clinician read (or speak) in unison. (Minimally useful technique, enables client to demonstrate change in his speaking process)
SLOW RATE - Patient speaks at a deliberate, steady, reduced rate. (Promotes relaxation and tension reduction; enables speaker more time to implement other speech targets; has almost universally beneficial effect of diminishing the number and severity of disfluencies)
SMOOTH SPEECH - Speaking in a manner that emphasizes the continuity of speech; generally at slightly reduced rate with forward ballistic movement. (Emphasizes the sensation of continuous movement and transitions from syllable to syllable and word to word)
PAGE 13
SOFT VOICE - Using significantly less intensity and muscular effort initiating voice and continuing to speak. (Develops relaxed control of voice onset and speaking voice)
SYLLABLE STRETCH - Elongating the voiced component of a syllable during speech; often for up to two seconds. (Slows rate; focuses attention on the volitional act of speaking; builds prosodic elements of speech and continuity of syllables)
VOLITIONAL CONTROL —> UNMONITORED SPEECH - Beginning the first few syllables or words of an utterance in a controlled manner, then "letting go" using spontaneous fluency. (Develops control of speaking, monitoring and "self-reinforcement")
VOLUNTARY STUTTERING (PSEUDO-STUTTERING) - Intentionally stuttering on words, imitating one's own or a different form of stuttering. (Desensitizes and discloses stuttering, enables volitional control)
WHITE NOISE OR MASKING - Noise is used at an intensity level great enough to impair the speaker's ability to hear his own speech. Some devices are "voice activated", turning on the masking as the patient begins to speak. Many view the device as "gimmicky" and yielding only temporary results. (Reduces auditory feedback, emphasizes oral proprioceptive feedback; some object to wearing the device; may serve as a means to diminish fear of stuttering)
PAGE 14
Therapy Skills
AN OVERVIEW OF THERAPY
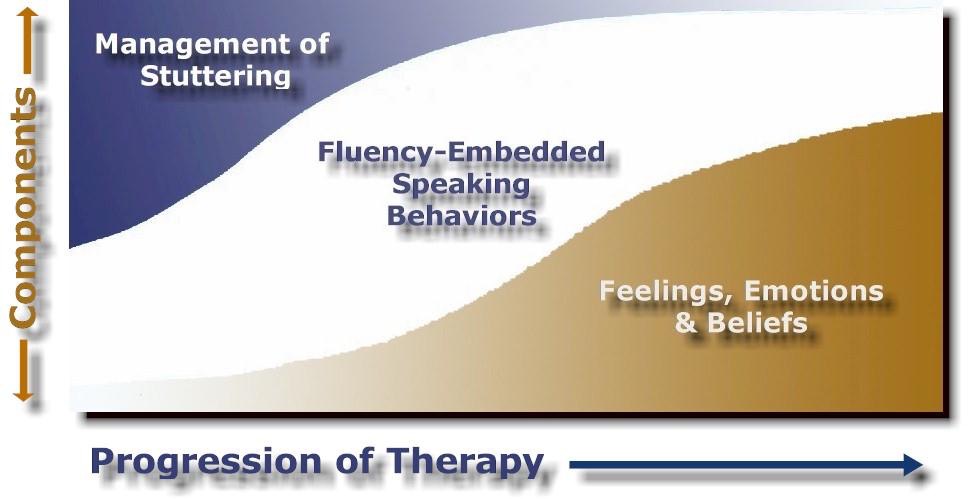
Overt and Covert Components. Successful treatment addresses the physiological and psycho-social aspects of stuttering. Establishing confidence in speaking fluently and overcoming the emotions, feelings, beliefs, attitudes, and behaviors that develop in response to stuttering are core components of therapy. These facets are interrelated and pursued concurrently in treatment. Therapy progresses along several dimensions and clients may work on different individual aspects of treatment simultaneously.
The physiological components (observable disfluent speaking behaviors) of stuttering are addressed by becoming better at managing stuttering moments and learning new, fluency-enhancing speaking behaviors. Therapy is, in part, symptom-specific, addressing core features of the individual's stuttering while forming new, more efficient speaking habits.
The psycho-social aspects (covert components) of stuttering are the reactions and behaviors that result from stuttering. Since many attempt to keep their stuttering a "secret", these feelings, behaviors, attitudes and beliefs deeply complicate and compound the problem. These covert components contribute strongly to the feeling that stuttering is "uncontrollable" and "unpredictable". For many, these covert features operate 'just below the surface', and their effects are not easily recognizable.
The course of therapy seeks to have each client:
- Better manage their stuttering
- Learn new, fluency-enhancing speaking behaviors, and
- Modify their thinking about stuttering and speaking
Managing Stuttering. Therapy usually begins by reviewing the normal process of speaking (describing respiration, phonation and articulation). This forms the basis for the client to learn to describe the overt attributes of their stuttering. With knowledge of their stuttering, the client begins to purposefully change the way they and begin to gain more and more control over disfluent moments.
Fluent Speaking Behaviors. Clients are also instructed to use speaking techniques (targets) that address the differences in their speaking patterns (the symptoms of their stuttering). These speech "targets" promote fluency, usually in a way that overcomes their habitual pattern of stuttering. By systematically "replacing" stuttering with fluency-enhancing speech targets, clients become more aware of their speaking differences and better able to speak in a way that results in fluency.
Emotions: Thinking and Feeling. The way each person thinks about their stuttering and speaking abilities has a strong influence on the severity, persistence, and degree to which stuttering handicaps their life. Consequently, discussing, challenging, testing, and modifying the client's thoughts, feelings, and beliefs about their stuttering is an important part of the therapeutic process.
These three therapy components are presented concurrently. But, as illustrated in the diagram below, the amount of focus on each component changes as therapy progresses. Therapy usually begins by working on ways to modify
PAGE 15
stuttering behaviors and begin to gain some control over disfluencies. As depicted in the diagram, this comprises the majority of effort in therapy, with some time being dedicated to fluency-enhancing skills, and only a little attempt to address feelings and emotions.
But as therapy progresses, more time is spent on speaking in ways that facilitate natural fluency and increased effort is expended to deal with the psycho-social issues of stuttering.
The overall approach is flexible enough to adapt to a client's experience with previous therapies, or work to build a new treatment regimen to support them. Therapy begins at the level of the client's current abilities; progress develops at the pace of the individual.
With adolescents and adults, habits usually develop that contribute to the severity of stuttering behaviors. The strength of many years of habit patterning is difficult to overestimate and often represents a considerable obstacle to transitioning controlled fluency into speaking situations perceived to be stressful. It may also contribute to relapse. Many have never developed a normal sense of communicating and find even simple conversations awkward and threatening.
Fluency is not usually the anticipated terminal goal of therapy, but merely a direction toward achieving confidence and competence as a successful communicator. The end product of therapy is to enable the client to appropriately participate in any communication situation encountered in activities of daily living. Clients also need to be prepared to handle relapse and the day-to-day fluctuations in their fluency. Many go on to redefine themselves as communicators, reshaping their self-image and self-perception as a confident and competent speaker, even in the most challenging situations.
THE COMPONENTS OF THERAPY
Speech Aspects of Stuttering Therapy
Awareness - Therapy begins with a review of the normal process of speaking (respiration, phonation, and articulation). The client is then led to identify each disfluency and later describe the type, place, and duration of the disfluency.
PAGE 16
Speech Change - The client generally effects changes in their stuttering using stuttering modification and fluency enhancement approaches. Stuttering modification may consist of stretching out a block (while releasing the tension), bouncing through a block, or stuttering in a different way than is their regular habit. By learning to alter the existing stuttering, clients learn to modify and then minimize their disfluencies, which gives way to lessening the severity, and eventually, beginning to control stuttering. Fluency enhancement approaches "re-pattern" the client's speech to be more consistent with normal, efficient speaking processes; these usually emphasize breath stream management or voice onset. The purpose of the Speech Change is to weaken the old habit pattern that results in stuttering, learn that one need not be held 'captive' by a disfluency, and begin to release the excess tension used in the articulatory process. This involves the client's implementation of targets in advance of (in preparation for) stuttering.
Preparation - Speech targets are selected based upon the symptoms of the client's stuttering. Targets promote fluency by countering the maladaptive aspects of the speaking process in the stuttering pattern. Targets are used in preparation for speaking fluently. Thus, it is incumbent upon the client to take responsibility for being fluent (compensating for their habits that precipitate stuttering). Both Speech Change and Preparation progress through a hierarchy of difficult/stressful speaking situations.
Habitualization Eventually, the number of speech targets is reduced to one that serves to bring all aspects of fluency together - the Keystone Target. The Keystone Target simplifies the encumbrance of using multiple targets, allowing the client to shift more resources to the content of his communication more easily. As confidence builds, emotions are excited less often and excess tension during speaking diminishes.
Emotional Aspects of Stuttering Therapy
Awareness - For some, the pain of stuttering is so great that they shut down their emotions as a means of self-protection - they allow themselves to feel no pain and are unwilling to acknowledge it. This is not a healthy situation. Confronting the pain can be a delicate and painful experience in therapy, but nonetheless a very important one. Awareness may begin in recognizing the physical symptoms elicited when emotions are set into play, learning the client's signs of anxiety and tension. Others may be more open to sharing their feelings and their emotions may be labeled and discussed more easily.
Identification - Learning which emotions are brought into play by stuttering and the meaning of these emotions can be a starting point for discussions. Group discussions, composed of people who do and do not stutter, may be useful in highlighting commonalties and differences in feelings about speaking among people who stutter and among all people. Identification of emotions enables the clinician to build a composite of the client's attitudes and beliefs about stuttering that underlies much of their maladaptive behaviors and habits.
History - Discussing details of childhood and adult experiences in which stuttering has played a part is helpful in revisiting those experiences and addressing them now with adult coping skills. Telling the story of one's injustices relating to their stuttering is therapeutic in being able to revisit them as an adult and gaining the understanding with the support of others. Modification and Implementation - Maladaptive beliefs about speaking are challenged to force the client to reorganize his or her attitudes and self-perceptions. Like speech targets, the client engages speaking situations with reality based emotional targets as well.
PAGE 17
Integrating the Aspects of Stuttering Therapy
Clients learn that the new speech and emotional targets can be integrated to reduce the fear, anxiety and avoidances that increase their muscular tension, and diminish their cognitive abilities to better monitor their speaking, and use speech techniques. Habit pattern strength is gradually diminished and new, more productive habits replace the old, maladaptive ones. The benefits generated by this combination empower the client to manage his or her fluency and maintain responsibility for it.
TASK MODES IN THERAPY
The task activity in therapy is a variable that can be used to increase or decrease the difficulty of the task for the client. The following information provides a few insights into the use of speaking modes to promote learning new techniques and challenging emerging skills.
Reading. For most clients, reading is less demanding than speaking as the words, lexicon and ideas are already represented in the text being read. However there are exceptions. Some clients experience reading difficulties that add to their disfluencies. In these instances, reading should be used sparingly or materials selected that are skill appropriate. For others, written materials obviate the clients use of avoidance strategies, substituting other words for those that are perceived as likely to be stuttered.
Reading, however, is a good starting point for most clients. The majority of clients are able to read aloud with significantly less disfluency. For these clients, it is suggested that short articles be selected, followed by a discussion or summary of what was read. One idea is to clip "Dear Abby", "Ask Ann Landers" or "Miss Manners" articles from the newspaper. Paste the letter on one side of an index card and the answer on the other side. Have the client read the letter aloud, then provide his or her own answer. Then read the columnist's response aloud. The blend of reading, speaking and reading again can be used to flow from a strength (reading) to a 'challenge' (spontaneous speech) and back to a 'strength' again. This can help the client transition their skills from one mode to another.
For clients who have more disfluencies reading, having a prepared text enables the clinician the advantage of knowing what the client is attempting to say, making it easier to provide instruction. Reading can be used to identify and analyze disfluencies and as an activity to implement speaking targets. Clinicians are encouraged to give clients feedback immediately as they read, stopping them when necessary. Clinicians should not wait until the client is finished reading a whole paragraph before instructing them in ways of improving their technique. Many clinicians have a tendency to advise clients on several types of 'errors' they make. It is better to focus on one or two speech targets at a time, rather than mix too many together.
Using slow rate as a target, reading in unison with a client can also serve as a means to guide the client to find the rate desired. Clients often tend to go faster than is optimal, and reading aloud in unison helps establish a slower rate.
Monologue. While some clients are very talkative, others are exceedingly quiet. Many adults who stutter have not had much positive experience talking and are very used to being verbally introverted. Adolescents too may prove to be reluctant to speak. For others, stuttering is more an annoyance or a frustration in getting across the things the client wants to communicate. With these scenarios in mind, using a monologue task may or may not be appropriate.
For those reluctant to speak, the clinician should not ask questions that can be answered with "yes" or "no." A picture description task or giving directions to a local landmark may be more effective in generating utterances.
PAGE 18
Clients reluctant or unable to volunteer a sufficient number of responses should be moved to reading tasks. Clients who are more verbose may require frequent interruption and direction. Some clients do not always discern that, in therapy, clinicians are more concerned with "how" things are said, than "what" is said. (In counseling sessions, however, just the opposite is true.) Inexperienced clinicians are often reluctant to interrupt a client before they complete what they are saying. However, a great deal of therapy time is "wasted" by allowing the client to stutter on word after word, not attempting to use any of their targets. Intrinsically, clients understand that it is the clinician's job to monitor his speech and provide feedback. As clinicians mature they learn to diplomatically stop the client, give instruction and resume the monologue. The objective of the task should be foremost in the clinician's mind in managing a client's speaking behavior.... maximizing the number of successes in each task. The length of monologue tasks is an important variable; begin short, expand the length of the monologue to correspond with the client's rate of success.
Conversation. Conversations are usually more demanding tasks, as they allow little time to formulate and reply to the partner's verbal response. As such, managing a slower rate of speech can be a vital component to the client's success. Also, emotional topics, such as 'abortion', may evoke strong feelings that need to be expressed; these compete with the client's ability to self-monitor and use speech targets. Nonetheless, such topics provide challenges as clients become more skillful.
Conversations enable the clinician to model targeted techniques while conversing with the client. Later, the clinician may use hurrying, disinterest, inattention, and interruptions to challenge more advanced clients.
Conversation is also a mode to transition from the clinic to other environments. Engaging strangers in conversation, speaking with co-workers and conversing at social gatherings are activities that many people who stutter find stressful. As such, group therapy or stuttering support groups may pave the way toward transitioning to real-world experiences. These real-world encounters frequently represent a big step and as such, clients initially regress in their skill level.
Presentation. One of the most common stresses for virtually every speaker is presentations. A presentation is most like an extended, prepared and rehearsed, formal monologue. In my experience, a therapy assignment to make a presentation at the next treatment session, usually results in an excuse: "I forgot." or "I didn't have time." This most often actually means "I was too frightened to do it." Often the client needs to do a presentation at work or at school and is suddenly 'highly motivated' to work on their talk. Unfortunately, the big presentation is usually the next day or in a few days, leaving little time to make any truly constructive improvements. It is the clinician's discretion whether to try to work on it or not. Attempting to prepare the client for something way over their head most often has no impact, and the client's feelings of "this doesn't work" are again reinforced. It may be more appropriate for the clinician to say, "This requires much more work than we can do in the few days available. We can, however, begin today to prepare for the next talk you will need to give, but there is very little we can accomplish at this date. We need to learn from this experience and devote more time into preparing for future speaking occasions."
Spontaneous presentations are good activities. One goal is to become more relaxed while in the role of "the speaker". Presentations should be long enough to have the client experience the anxiety and feel it dissipate while standing before the group. Learning to be more comfortable in the speaker's role comes from multiple opportunities, in several different environments. Moving outside of the client's comfort zone elicits feelings of fear, excitement and opportunity; the key ingredients of change and improvement.
Telephone. Most clients who stutter commonly fear the phone. Many express concern that all the listeners attention is focused on their speech because they can't be seen as they talk. This attention increases the client's fear and tension, which increases their stuttering behaviors
PAGE 19
Another significant issue in using the phone is the time it takes the client to initiate speech once the other party picks up. Listeners can be very impatient when it appears no one is on the other end of the phone or the thought that it is a "crank call". Listeners wait only a few seconds before hanging up...an experience the client has likely encountered countless times before. This time pressure is typically very difficult for people who stutter and usually precipitates stuttering blocks. With this pressure, the clients don't realize how much they change their speaking pattern when attempting to use the telephone. Just the thought of making a call stirs emotions and physical changes in the process of speaking.
Thus, phone calls often begin with desensitization tasks; stuttering voluntarily to the phone partner while asking the store hours. As the client becomes less fearful and better able to initiate their voice, continued practice results in smoother, softer initiation of speech. Attention needs to focus on the changes made in the normal, fluent speaking process when confronting phone calls. Often, breathing becomes shorter and more rapid. Typically, clients take a deep gasp immediately before trying to phonate, almost insuring they will block. As awareness builds, the client begins to see the pattern that leads them into stuttering. With the clinician's guidance, they begin to implement their speech targets and eventually overcome their difficulty speaking on the phone. For most, it is a long and difficult struggle.
In General. Talking with your client enables the clinician to begin to learn their feared situations, words and sounds. In the vast majority of cases, the client's pattern of speaking changes dramatically in these feared situations, most often without their awareness. The clinician should not always accept the client's reassurances that particular situations to not present difficulty, as some clients attempt to mask their fears with bravado. A few actual phone calls will reveal the client's actual abilities. Someone who doesn't find phoning difficult shouldn't mind making a few calls.
USING HIERARCHIES IN THERAPY
Most clients report that some speaking situations represent bigger challenges than others in terms of their fluency. The specifics of this information are very important in designing therapy because clients usually begin using their targets in speaking situations that are less difficult, and work along through situations that are progressively more taxing.
Consequently, one of the first things clinicians need to do is work with their client to establish a list of speaking situations that are difficult for them. Next, the situations are arranged in a hierarchy (a sequence from least to most difficult). This is accomplished by talking with the client to learn when their stuttering is more pronounced. Some clients find it difficult to articulate their difficult speaking situations; the clinician might then suggest scenarios for the client to respond to. These might include speaking to their boss or an authority figure, giving a presentation to a large audience, speaking in a noisy environment, answering the telephone, making a phone call, leaving a message on an answering machine, making introductions, making an appointment with a doctor's office, interviewing for a job, speaking with someone who is angry and so on.
Sisskin (2002) suggests constructing communication hierarchies based upon four parameters; where, who, what, and when. Where describes the environmental context of the communication - at the office, in the waiting room. Who depicts the person or group of people - my boss, my parents. What delineates the type or form of communication - conversation, reading aloud. When refers to the particulars of a situation - when angry, when rushed, when nervous. Clinicians can create a hierarchical matrix to guide planning of the client's treatment sessions.
Patient progress can be monitored by tracking the level of success the client achieves as he moves along the dimensions of their hierarchy.
PAGE 20
Note: Clients are often perplexed and disappointed by the difference in their performance levels between working in the clinic and practicing in other situations. The therapeutic environment is often perceived as a magical place where their targets seem to work much better than after they leave. It is important for the client to understand that the ideal conditions of the treatment room are much different (by design) than the real world. Clinicians can use their hierarchy as a way to explain this phenomenon and help the client understand and prepare for the challenges that other situations present. I sometimes tell clients that their ability in the therapy room is a window into the future and that, with practice and perseverance, they will soon be able to do equally well in other environments too.
Source: Sisskin (2002), Therapy Planning for School-Age Children who Stutter, Seminars in Speech and Language, 23, 173-180.
GIVING HONEST FEEDBACK
It is difficult, but essential, to provide honest, objective feedback regarding your client's performance when they have not succeeded to the degree you or they might reasonably expect. Many clinicians feel they are being supportive by withholding or "sugar coating" objective analysis of a client's performance. But by not being objective, clinicians undermine their credibility by overlooking unsuccessful attempts in therapy. The design of therapy is not to be successful all the time. In fact, that is an indication that the treatment objective is too easy for the client and that the clinician is failing to push the client hard enough. Effective clinicians help their clients evaluate and judge their own successes and failures. In the therapeutic relationship, the clinician needs to establish a clear objective and assess each attempt in an impartial way so the client clearly understands what is expected.
Three general approaches are offered to assist clinicians in communicating feedback objectively and tactfully to clients.
Direct Approaches: Clinician initiates, giving information specific to the event.
- 1. Direct, to the Point — Work with the Client's Reaction
- Clinician: "You didn't use your targets!"
- Client: "I know, but I tried."
- Clinician: "When were you first aware you weren't using them?"
- 2. Drop and Fix
- Clinician: "You were speaking too fast; let's try to slow your rate next time by only speaking when you have initiated eye contact."
- 3. Plus Two, Minus One
- Clinician: "I saw good airflow; I noticed good eye contact; but it seemed you hurried too much."
- 4. Objective-Based Feedback (Separating the behavior from the person.)
- Clinician: "I noticed that the airflow didn't start early enough."
PAGE 21
Semi-Direct Approaches: Feedback is provided by relating it to the event; seeks to elicit the client's initiation of the topic
- 5. Self-Assessment
- Clinician: "What did you notice happened that time as soon as you began talking?"
- 6. Comparative
- Clinician: "How did that differ from your success at the meeting?"
- 7. Re-Take
- Clinician: "If you could do that again, what would you do differently?"
- 8. Instructive Re-Focus
- Client: "My targets didn't work!"
Clinician: "It seemed in this situation we need to work more on preparing to use your targets earlier."
Indirect Approaches: Clinician shifts focus of feedback to another aspect of the event
9. Refocus
Client: "My targets didn't work!"
Clinician: "It must be very frustrating being able to do it some times and not at other times."
-
10. Indirect
Client: "My targets didn't work!"
Clinician: "I've seen things to have worked better for you in other situations."
Pragmatics of Presentation
Attitude: The clinician expresses the following attributes through their attitude — a solid belief system (the way they think about stuttering and fluency therapy), honesty, sensitivity, goal-orientation, respect, sincerity, sense of importance and urgency, and directness.
Word Choice: The clinician selects words that succinctly, directly (not vaguely), matter-of-factly, consistently and tactfully enumerate how a behavior varies from the expectation.
Body Language: The clinician purposefully maintains eye contact with the client; their body posture is slightly relaxed so as not to be perceived as threatening or attacking; gestures and facial expressions are used to communicate sincerity, directness, and objectivity.
A Few Last Words
Artfully critiquing a client's performance is a skill that develops with time, practice, and experience. Clients will respect your honesty, even when it directly identifies their flaws. Honesty builds trust in a therapeutic relationship. As a clinician, your first responsibility is to facilitate your client's improvement. It is nice to be liked by your client, but it is not imperative, and certainly secondary to success in therapy.
PAGE 22
MAXIMIZING TEACHING EFFECTIVENESS IN THERAPY
To get the most from each therapy activity, consider taking advantage of the three teaching opportunities you have by (1) explaining the activity you are about to do and the part it plays in the overall treatment plan for the patient, (2) providing feedback during the activity, and (3) summarizing the patient's performance at the conclusion of the activity and providing direction for the future by explaining the next step that they are heading forward.
Setting the Stage. Activities afford the client situations in which to practice their targets, and are usually planned along a hierarchy of difficulty for the client. Clients learn better when they understand and more fully appreciate what they are doing and why. Begin by describing what you wish the client to do for the therapy activity; then why it is important, and how it fits into the scheme of their therapy plan.
Example: "Now I am going to have you share your opinion of the movie you told me you saw last weekend using your slow rate target. You have done very well maintaining your rate in reading, but a monologue is more challenging because you need to think about what you are going to say and how you are going to say it. This activity is important because in our everyday lives we are much more likely to express our opinions verbally than read aloud. Because this is more challenging I expect that you will have to focus harder on using your targets. Now, what did you think of the movie?"
Providing Feedback. Giving immediate feedback is important for the client to learn to use a target appropriately, evaluate their own production, and make adjustments. At the beginning of an activity, you might initially flood the client with feedback, providing both positive assurance and corrective suggestions for the first minute or so.
After a minute, back off and see how the client does on their own. Then provide additional feedback as needed. Periodically let the client know when they've been successful.
Imagine that I am a passenger in a car that you were driving; you are blindfolded. How often would you want me to give you feedback about your driving and upcoming obstacles? Would you only want to know when a problem was approaching or would you also like to know that everything was okay as well?
Example. "You're off to a good start..... That's exactly right..... Good..... You're speeding up a little now... Watch it... Right!.... How is your rate right now? [Don't hesitate to "talk over" the client as he is talking.]
Summative Feedback. At the conclusion of an activity put the client's performance in perspective. Share your honest opinion of how they did; respect them enough to tell them when they did not do an adequate job and explain why. (See "Giving Honest Feedback" for suggestions.) Critically analyze the client's performance, acknowledging what they've done well and providing constructive suggestions on how to improve further. Lastly, paint the bigger picture of where they are along the continuum and where they will be going next.
Example. "Hey, that was the best job you've done so far; you maintained your slow rate target very well. I noticed that you did better initially, but then seemed to speed up a bit after about two minutes. I saw that you were monitoring yourself, because there were three occasions I heard you purposefully slow your rate again. That tells me that you are taking the responsibility to listen to yourself and make the necessary adjustments without me
PAGE 23
pointing them out to you. That's great progress. I'd like to practice that in our next session and for you to continue to work on that at home and the office. It's likely going to be more difficult when we choose a topic that you have strong feelings about, so I'll plan to incorporate that into our session next week too. As you continue to improve on using your target on your own, I want to move you into situations that are more and more challenging, so you'll continue to grow. I'll be looking for you to demonstrate the same kind of monitoring and adjustments you made in this activity today; but the skill I'd like you to master is pacing yourself consistently throughout the entire conversation."
Getting the most out of each activity is a therapist's obligation. Using these suggestions will also make you think more about what you are doing and where you are taking your client. They also facilitate better communications between you and the client.
TEN SIGNS OF PROGRESS IN THERAPY
Progress in stuttering therapy is not always obvious; it is often not measured by a reduction in the frequency of disfluencies, but more subtle aspects of behavior and cognitive awareness. As clinicians become more familiar with their client and with the disorder of stuttering, signs of progress may be found in several dimensions. The list below offers some areas in which to look.
- 1. Awareness of the Core Features and Secondary Characteristics of Stuttering
- The client's ability to accurately identify the elements of his core features of stuttering and the secondary behaviors they evidence. Persons who stutter typically block awareness of their stuttering because it is psychologically painful to experience. Thus, growth in the objective awareness of stuttering indicates a willingness to let down psychological protective shield and be more open and objective.
- 2. Changes in Stuttering Behaviors
- Any change in or modification of the chronic stuttering pattern represents an opportunity to break down the habit patterns that have become so strongly ingrained. Changes might be found in modifications of core features of stuttering, such as bouncing on a disfluent sound instead of blocking on it.
- 3. Mastery of Speech Targets/Techniques
- The degree to which a client can successfully demonstrate a therapy target or fluency technique in progressively more difficult modes of speaking.
- 4. Control of Stuttering
- The patient's ability to modify and gain control over a core stuttering behavior while speaking.
- 5. Fear of Stuttering
- Reduction in the degree to which fear of stuttering adds to the client's tension level, interferes with their confidence and their ability to effectively access speech targets.
- 6. Use of Targets in Stressful Situations
- The ability to utilize or attempt to use techniques in increasingly more challenging speaking situations. This demonstrates the client's emerging ability to manage the 'fear' signals learned from past experiences.
PAGE 24
- 7. Openness of Feelings
- The ability to access and discuss feelings about self and stuttering. This signals the willingness to bring down protective barriers and begin to address the emotional components of their stuttering.
- 8. Effecting Fluency
- The ability to transition from stuttering modification to fluency shaping/enhancement techniques. This emerging and fragile skill generally demonstrates a generally upward progression, with peaks and dips of success along the way.
- 9. Responsibility for Change
- The client looks inward to create fluency, rather than perceiving external factors as being responsible for their disfluencies. Clients no longer see themselves as a victim, but as being empowered to affect their fluency.
- 10. Confidence as a Communicator
- The individual looks beyond fluency as the measurement of their success as a communicator. He evidences greater poise and self-assurance in speaking situations and their personality is reflected in their speaking style.
EXPLAINING STUTTERING
One of the complicating factors in stuttering is that its cause has yet to be determined. This is pertinent for two reasons. First, most people are naturally interested in understanding all they can about the nature of their malady. The cause of stuttering has been the focus of research for many, many years. Some theories of stuttering imply less than flattering things about people who stutter. For example, one persistent thought posits that stuttering is the outward manifestation of a deep-seated emotional problem. While there is no research to support his speculation, remnants of this supposition persist and serve to perpetuate elements of the falsehood. For instance, in the International Classification of Diseases (ICD-9), stuttering is listed under Neurotic Disorders, Personality Disorders, and Other Non-psychotic Mental Disorders. Imagine the impact of feeling that others are thinking of you as having an emotional problem, when you don't!
The other issue relating to discussing the cause of stuttering deals with framing the person who stutters as the expert, educator, and dispenser of knowledge about stuttering. Being able to discuss your stuttering with others makes a statement about your feelings about it and how it affects you. People unable or unwilling to talk about their stuttering leave the impression that it is a really bad and shameful thing; consequently, others are unlikely to broach the topic and often feel sympathy or pity for the person with such a weighty problem. People able to talk openly about their stuttering are seen as knowledgeable and maintain their dignity, because they project an objective attitude toward their stuttering. Talking about it engages others interest. Directly the opposite of the person who stutters fears, others are drawn to become supporters, rather than critics. Think about how you would respond to someone who is notably overweight, holding his head down, unable to make eye contact with you, and not eager to interact with others. Now, compare that to another overweight person who engages you in a conversation about why he has gained weight, and excitedly tells you about the new diet and exercise program he has started to get to his ideal weight. Which person are you more likely to feel sorry for and which person do you want to help and provide encouragement.
PAGE 25
Talking about stuttering in an objective, knowledgeable way enables the person who stutters to appear on top of the problem. But how can you speak in a knowledgeable way about a problem when even the scientists don't know the cause?
Knowing the real cause is probably less important than believing in a cause and being able to talk about it intelligently. (After all, that is what the professionals do!) Work with your client to develop a script that they can use to talk with others about the cause of their stuttering. Try to include some research to support their beliefs. In my experience, the process of preparing and rehearsing how to talk about stuttering helps clients crystallize their feelings and beliefs. It seems to give them a sense of strength and stability and helps develop self-respect.
A sample explanation appears below and may serve as a starting point for clinicians in developing a script. The clinician's role in this task is as a facilitator, drawing out, guiding, and supporting the thoughts of the client.
Stuttering is a complex problem. For some, stuttering seems to run in families, so there may be a genetic factor. Research using PET scans found that people who stutter use their brain in a different way when they speak. It seems when we stutter, we use both the right and left hemispheres to talk. There also seems to be less coordination between the hemispheres, without one hemisphere taking a 'leadership' or 'coordinating' role. As a result, the two sides of the brain that control speech don't work effectively together and the process of talking gets tangled up. Most of us who stutter find that we are less fluent in certain situations, like when in a hurry, speaking on the phone, or meeting someone for the first time. To compensate, I've been learning how to slow my speech down and start sounds at the beginning of a sentence easier. In fact, if you wanted to help me, you can remind me to go a little slower when you notice that I start going too fast. And, just give me a second or two more to get out what I want to say. It's annoying when people try to fill-in the words I'm trying to say for me. I know they are trying to help, but it throws me off and makes me feel like I've failed.
This script is relatively brief, but it also lets people know what they can do to help! It invites questions about stuttering and positions the person who stutters as the expert. As any speech pathologist will tell you, the person who stutters knows more about their stuttering than anyone else!
ANOTHER PERSPECTIVE ON THERAPY
Another way to think about stuttering therapy is to consider three elements of the overall process: Information Gathering, Building Fluency, and Structuring for Continuing Success. This premise is based on the following assumptions:
- People who stutter lack objectivity in evaluating their stuttering. Most have acquired misinformation (distorted perceptions) about their stuttering. Therefore, establishing a good information base about their stuttering is an important fundamental step.
- There are many ways to build fluent speech. No single way appears to work for everyone. The techniques used are probably less important than the clinician's ability to encourage the client to change his speaking habits in a direction that enhances fluency.
PAGE 26
- Rebuilding attitudes and repairing feelings are important components of laying a foundation for longterm success and continuing improvement. Many have gained fluency only to lose it later. Others struggle to be able to change habitual speaking patterns and find implementing therapy techniques to be a sincere challenge.
Information Gathering
It is important to learn general information about the normal processes of speaking and stuttering. There is considerable misinformation about the nature and cause of stuttering that often serves to needlessly complicate the client's ability to understand and cope with their stuttering. Knowledge is power.
Clients need to be able to identify the specifics of their own stuttering and see how the disfluencies of others who stutter are similar/different from their own. This may be accomplished by learning to:
- Identify the core behaviors of their stuttering and how it differs from and interferes with fluent speech production
- Recognize their secondary characteristics as they relate to core behaviors and their feelings and attitudes about stuttering
Building Fluency
Clients need tools to help them change their speaking patterns. Their attempts to control and manage stuttering have resulted in maladaptive habit patterns from which they are unable to escape. The clinician provides new, more productive speaking techniques designed to be more compatible with the goal of fluent speech. The fluency tools chosen need to be productive and acceptable to the client.
- In general, regardless of which fluency tool is utilized, the instructional paradigm for gaining control over stuttering and developing fluency patterning progresses through the stages of:
Identifying —> Modifying —> Control and Shaping Fluency
- Becoming desensitized to the fear of speaking and stuttering, as well as readjusting the self-perceptions of the person who stutters, are integrated with the speaking techniques.
- Each individual needs to assume responsibility for speaking fluently and for making changes
Structuring for Continuing Success
There are probably as many reasons for fluency therapy to be unsuccessful as there are people who stutter. Relapse is very common. Therefore, effective treatment programs must work to develop self-rescue skills to prepare clients for likely relapses in the future. Prepare the client to always be a person who stutters; it is unlikely to go away at this point in their life. The following ideas therefore, might benefit all people who stutter.
- Preparation - use focused, controlled speech as you enter your most difficult speaking situations; don't wait for disaster to happen; be prepared and plan to be fluent.
- Attitude - view speaking as rewarding; find satisfaction in communicating orally; define your success in terms of the information you communicate, rather than your fluency.
PAGE 27
- Challenges - actively seek out new speaking situations to maintain your current ability and development of new speaking skills; willingness to take risks. Like typing, the more you practice and use your skills, the better they become. The less often you use them, the rustier you get.
- Confidence - you can develop a sense of self-assurance while speaking; cultivate a sense of self, a personality, as a speaker.
- Spontaneity - increase your inflection and intonation as you gain more and more fluency; learn to reflect the new you in the way you speak.
- Relapses - in life, as in stuttering, not every day is a good day. Develop a plan in preparation for bad speaking days; network with others who stutter; become active in support groups; be self-reliant by being your own advocate and speech coach.
Stuttering is a complex problem with many facets. Adults and adolescents who stutter have come to learn many negative things about their stuttering; many have internalized these lessons. The process of becoming a successful communicator is lengthy and challenging.
PAGE 28
Fluency Techniques
Note: to activate the embedded YouTube video clips in this section, you may have to hit the start icon at the beginning of the video twice.
There is a core group of speech therapy techniques (targets) used in the vast majority of treatment programs for stuttering. These speech targets are described below.
Generally, clients focus on one or two speech targets at a time in their therapy. Occasionally the targets are used consecutively in the course of therapy, but most commonly they are used concurrently. When techniques are employed concurrently, the transition from one target to practicing another target needs to be clearly delineated for the client.
Targets are generally selected based upon the treatment philosophy of the clinician, the target's applicability to the specific symptoms of the clients stuttering, the client's willingness to use the target, and the effectiveness of the target in enhancing speech fluency. Further explanation is provided below.
Philosophical Considerations. Some clinicians operate from a specific ideology or theory of how stuttering behaves. Other clinicians are more eclectic, and their selection of targets is more strongly influenced by other factors. In either case, the clinician needs to be able to explain their rationale for their selection of techniques used in therapy to the client. It is important that the client understands how what he is being asked to do works.
Symptomatic Considerations. Targets are usually selected because they address a specific stuttering symptom evident in the client's stuttering. For example, when a client demonstrates excessive force articulating plosive sounds, a 'light articulatory contact' may be chosen to correct this aberrant characteristic of the client's stuttering. If a client has many symptoms, only one or two targets are selected for use for a period in therapy to better enable mastery of each target, before moving on to others.
Effectiveness Considerations. Effectiveness is usually a function of selecting a technique that remedies the specific symptoms of stuttering. However, it is also dependent upon the client's ability to master and utilize a technique effectively. Generalization is a related consideration. One or sometimes two targets often emerge that have a "spillover" effect. That is, one technique may prove beneficial to other symptoms or aspects of disfluency, beyond the specific symptoms of the target addresses. This "keystone target" usually becomes the primary focus of later therapy.
COMMON SPEECH TARGETS IN STUTTERING THERAPY
There are two general categories of fluency targets those designed to enhance fluency (fluency shaping) and those that teach the client how to modify his stuttering. Both approaches (fluency shaping and stuttering modification) are important skills for clients to be able to manage their fluency and control their stuttering. Fluency shaping skills are based on principles of normal speech production whereas stuttering modification skills enable the client to better manage (minimize) his existing stuttering disfluencies.
Airflow Technique (Fluency Enhancement)
Description: A deep breath is inhaled. Passive release of air (exhalation) is begun just prior to softly adducting the vocal folds to initiate phonation.
Symptom Relief: Laryngeal blocking and overall reduction of tension
PAGE 29
Benefits: Promotes relaxed breathing, tension reduction, eliminates excess muscular tension upon phonation
Therapy Tip: Begin instruction with a review of the basic anatomy and physiology of respiration and description of the movement of the vocal folds for phonation. First, practice inhaling to feel the expansion of the lungs and chest. Then, demonstrate exhaling to build proprioceptive awareness of the breathing process. Be sure the patient takes notice of the point at which inhalation stops and exhalation begins.
Next, begin phonation by gently saying "ah", highlighting the sensation of the vocal folds coming together and beginning to vibrate. Have the patient put their fingers on the thyroid cartilage ("Adam's Apple") to feel the vibrations.
Finally, instruct the client to allow more air than usual to escape before bringing the vocal folds together to phonate. Have them listen for an audible exhalation of air before voicing begins.
To establish their competency in using the technique, instruct the patient to read to short phrases using exaggerated airflow at the beginning of each utterance.
Watch a YouTube video of the Airflow Technique at: https://www.youtube.com/watch?v=ZEwYs9wlmx4
Light Articulatory Contacts (Fluency Enhancement)
Description: Emphasis is focused on a placing only minimal pressure at the point of contact made by the lips, tongue, teeth and palate during articulation.
Symptom Relief: Reduces excessive muscular effort used while articulating phonemes: this is often most pronounced on plosives or other sounds that obstruct airflow in the oral cavity. It may also be effective in managing repetitions.
Benefits: Promotes the appropriate amount of muscular effort while articulating, builds proprioceptive feedback of the speaking process, develops oral-motor awareness, and slows rate of speaking.
Therapy Tip: Begin instruction with a review of the basic anatomy of the articulatory structures, being sure to cover the major structures and landmarks, as well as common points that come into contact when articulating sounds. Have the client make a few sounds in isolation and ask him to describe the contact points used in producing the sound. Briefly explain some of the various ways the airstream is managed at the point of contact (for example, plosives, fricatives, etc.) to make sounds.
Point out to the client that only minimal muscular effort is needed to make the contact. The contact can accurately be made using only a very soft touch.
Have the patient read a few sentences, emphasizing the softness (lightness) of their articulatory contacts. Designate this speaking technique as a "Light Contact" so the client can affix the label to his speaking actions.
Next have the client read a sentence using "effortful articulatory contacts", then re-read the same sentence, contrasting it with light contacts.
See a YouTube video on Light Articulatory Contacts at https://www.youtube.com/watch?v=N4ldvmiShK0.
PAGE 30
Syllable Stretch (Fluency Enhancement)
Description: Words are articulated by stretching (prolonging) the vowel sounds by two full seconds.
Symptom Relief: Reduces rate, focuses on articulatory aspects of speaking, increases the amount of vocalization in words.
Benefits: Improves focus on the motor act of the speaking process, promotes volitional control of speech, reduces articulatory effort, slows rate of speaking.
Therapy Tip: Begin by preparing list of words that do not begin with plosive sounds. Highlight the first syllable of each word. Instruct the client to prolong the first sound of the first word, stretching it out for at least three seconds (exaggerated form), before completing the rest of the word.
Emphasize the relaxed nature of the oral musculature in stretching the sound and the movement from one sound to the next when articulating the words.
Some clients have difficulty at first as they begin blocking on the first sound. Try reading and stretching on the words in unison — reading the list of words together with the client.
Aim to build the feel of speaking in a manner that stretches the sounds. Proceed to reading sentences, stretching the words as you go along. Next, try a brief conversation in which both you and the client stretch the initial sound of words.
Gentle Vocal Onset (Fluency Enhancement)
Description: Voice is initiated very softly with a gradual increase in intensity. There is often a very brief puff of exhaled air that precedes the gentle adduction of the vocal folds. As phonation begins, intensity is gradually increased in a controlled manner.
Symptom Relief: Reduces excessive muscular effort initiating phonation, thus diminishing laryngeal blocks.
Benefits: Diminishes laryngeal blocks, builds volitional control and awareness of phonatory onset and modulation.
Therapy Tip: Review the basic anatomy of respiration and description of the movement of the vocal folds for phonation. Practice inhaling and exhaling; identify the precise point at which breathing changes from inhalation to exhalation.
Ask the patient to demonstrate a few breathing cycles. Next, begin phonation by gently saying "ah", highlighting the sensation of the vocal folds coming together and beginning to vibrate. Have the patient put their fingers on the thyroid cartilage ("Adam's Apple") to feel the vibrations.
Inform the patient that the vocal folds come together to begin to make the voice only an instant after beginning exhalation. Now, instruct the client to inhale, exhale, and then begin phonation later than is regular. Be sure that the vocal folds come together very softly and easily. Draw the client's attention to the sound of the air being exhaled between the time he or she begins to exhale and starts phonating. Ask him or her to accentuate that sound of the air escaping, so it is audible to you and the client. You might prepare a list of words beginning with vowel sounds. (It should sound as though the client is articulating
PAGE 31
the word beginning with an "h" sound; so he or she would actually say "harm" when attempting to say the word "arm" using the airflow technique.) Draw the client's attention to the easy onset of the vowel sound following the exhaled air.
Have the client read a list of single words beginning with vowel sounds to establish the technique. Later, move into a conversation task, in which both you and the client use the technique.
Slow Rate (Fluency Enhancement)
Description: There are several approaches to control speaking rate. The goal is to speak at a steady, reduced rate. Approaches may include using pacing (syllable or word tapping) techniques, targeting a rate modeled by the clinician, using a delayed auditory feedback device, or any technique that increases the volitional control of the act of speaking. The goal is to establish a new kinesthetic and acoustic model for speaking.
Symptom Relief: Most people who stutter experience dramatic improvement in most aspects of their fluency just by speaking more slowly. It is almost as if their speaking system (the ability to generate sentences, retrieve words, coordinate phonation with articulation, etc.) was designed to perform optimally at this slower rate, and that breakdown occurs when the system is pushed to go too rapidly.
Benefits: Promotes better control of the process of speaking, reduction of anxiety (a sense of being more relaxed), and a reduction in many types of disfluent behaviors.
For some it is a matter of (mis)perception. Listening to a recording of themselves speaking at a "slow-normal" rate sometimes leads them to realize that it doesn't "sound as slow as it feels"; they will use the technique effectively to their benefit. Rate is very difficult to change; clinicians should try to slow their own rate in a conversation with a friend to develop an understanding of the difficulty involved. Nonetheless, rate control is a "key target" that is most often used in specific situations by speakers in stressful situations, such as when giving a presentation.
Therapy Tip: A speaker's rate is often a reflection of the underlying anxiety he feels. Altering the "habitual rate", especially under stressful speaking conditions, usually results in the speech feeling very "unnatural". Most clients express that the slow rate sounds and feels abnormal, particularly at first when the target rate is at its slowest. Changing any established behavior is most difficult in stressful situations. Be prepared to convince your client that he should give this technique a fair try in a "safe", clinical environment, before discarding it altogether. Rate is very difficult to change; clinicians should try to cut their own speaking rate in half in a conversation with a friend to appreciate their client's experience.
For a few, the unnatural feeling of slow rate is a misperception. Listening to a tape recording of their speech at a "slow-normal" rate leads some to recalibrate and realize that it doesn't "sound as slow as it feels!" However most clients persist in their protests.
Rate control has a very pronounced, beneficial effect on fluency. It is often used as a "key target"; a speaking target that brings all aspects of speech production together to improve fluency. As beneficial as rate control is, almost all clients struggle to be able to implement this target. Your persistence in building your client's ability to better manage their rate is a vital component to building a collection of therapeutic tools.
See YouTube videos on Slow Rate at https://www.youtube.com/watch?v=0BzSeltJhns and at https://www.youtube.com/watch?v=Cpaa2vGazzE.
PAGE 32
Continuous Phonation (Fluency Enhancement)
Description: In normal speaking, the voice is used in producing some sounds, while not used for others (voiced vs. voiceless sounds). In a sense, fluency for some who stutter may be disrupted by the process of constantly switching between voiced and unvoiced sounds. With continuous phonation, the voice remains on as much as is feasible. Singing or chanting may be considered variations of this technique.
Symptom Relief: There is usually a primary reduction of laryngeal blocks and often a secondary reduction of oral stuttering blocks.
Benefits: The client experiences a sense of the flow of continuous uninterrupted speaking. For many, the benefit is mitigated by the noticeably different sounds of their speech
Therapy Tip: Continuous phonation is much like singing or chanting, in which the speaker maintains phonation (voicing) for a much greater proportion of the time. Many people are reluctant to sing, so chanting might be a better starting place.
Have a list of several sentences prepared for the client. You should model each step of the technique to instruct the client. First, simply and softly say "ah" for about 15 seconds. Have the client imitate your production. Draw his or her attention to the element of voicing being "on" the entire time. You might ask them to place their fingers on their thyroid cartilage ("Adam's apple") to help them monitor.
Next, repeat the word "me" several times, while sustaining phonation. Again, have the client mimic your production. Then, move on to two-syllable nonsense words, such as "me-moo", repeating it several times while maintaining phonation. Again, highlight the sound and feeling of the voice being "on" the vast majority of the time.
You might next move to reading a sentence, such as "My name is Mary" following the previous pattern of modeling, imitating, and highlighting the sound and sensation.
Most clients comment on the lack of inflection or affect. You might next seek to add inflection while reading or speaking sentences. Draw the client's attention to the flow of speaking, the smooth, effortless movement and the resultant fluency.
Pull-Out (Stuttering Modification)
Description: In the middle of a stuttering block, the client "stretches" the sound they are "stuck" on, "sliding" the stuttered sound and blending it into the next sound.
Symptom Relief: Intervenes in the stuttering habit patterns of blocks and repetitions.
Benefits: Builds volitional control of releasing from a stuttered moment; develops a sense of empowerment in which the client may no longer feel the victim of his stuttering because they can now manipulate (modify) their stuttering.
Therapy Tip: Pull-outs are an effective tool in teaching a client to be able to modify stuttered moments previously perceived to be uncontrollable.
PAGE 33
Pull-outs begin as a "para-stuttering" event; that is they are implemented after the disfluency has begun. Pull-outs are used to work out of a stuttering moment, in which the client has previously been unable to modify or change in any way. This is usually because the client attempts to use more effort or struggle to release from the block. The pull-out offers a first experience in successfully disengaging from the grip of the disfluency.
When the client encounters a block, instruct him or her to stretch out of the block, gradually releasing the tension and struggle. It is usually helpful to practice first on words that are not stuttered upon to get the feel of the technique. Next ask the client to read a prepared list of words upon which they usually stutter, using the technique on each disfluency.
With time, pull-outs can be used prophylactically; thus becoming a "pre-stuttering" event. On sounds or words the speaker fears, he or she will stutter on, they are asked to implement the pull-out before the stutter is initiated. This serves to minimize the strength of the disfluencies before it is encountered. The client learns a tactic to replace the struggle and effort that has become his habitual response to the disfluency.
Freezing (Stuttering Modification)
Description: When the client begins to stutter, he is instructed to keep stuttering on the same sound in the same manner until the clinician signals him to stop. When the client begins to stutter, the clinician raises her hand (signaling the client to continue his stutter); after a while, the clinician lowers her hand and the client is allow to stop the stutter.
Symptom Relief: Freezing intends to allow the client to experience a stutter long enough to allow the disfluency to dissipate. By maintaining the stutter, it soon goes from being an involuntary to becoming a voluntary motor act.
Benefits: The client begins to realize that he can begin to manipulate his stuttering and that disfluencies, particularly blocks, lessen in strength as the client learns to struggle less. There is a distinct point at which the stutter only continues because the client is continuing it. It is voluntary at that point and, once a voluntary motor act, it can be easily terminated.
Therapy Tip: Clinicians often ask how long they should have the client freeze (continue his stutter). As a rule of thumb, have the client continue the stutter until he begins to smile. His smile signals that, Hey, this is a ridiculous thing to have me do! At that point he realizes that the only reason he is still stuttering is because you are asking him to. This means the stutter (the dreaded stutter) is no longer real and as such, it becomes a lighter subject. The experience is that it's not something that is happening to me, I'm doing it myself, which is a new phenomenon. It's sort of humorous because it seems so absurd to do this; but a little bit funny at the same time.
Bouncing (Stuttering Modification)
Description: Bouncing is similar to a voluntary repetition. It is used as a means of changing or breaking up the clients stuttering pattern. When the client has a block, bouncing can be used to free him from the stutter by breaking up the tension. After the client realizes that he is blocking, he begins to say the sound as a repetition, instead of a block, substituting one form of stuttering for another. The difference is that the bouncing is voluntary and, as such, the client can terminate the stutter at will. Thus the client learns to volitionally change his stuttering pattern. Later, after some practice using bouncing, the client may choose to employ bouncing in advance to avoid blocking on difficult words.
Symptom Relief: Laryngeal and labial blocks can be lessened as the muscular tension is broken up by repeating the sound, instead in increasing the muscular effort used in the block. The client develops a tool to modify this characteristic of stuttering.
PAGE 34
Benefits: The client develops a means of escaping from a block and changes his habitual pattern of stuttering.
Therapy Tip: Clients are often quick to point out that bouncing is still stuttering; however, there are a few important differences. Foremost, bouncing is intentional, not involuntary; the client is doing it on purpose. A block is involuntary and as the client adds effort and force attempting to fight through it, it only gets stronger and the client remains stuck! Second, bouncing is a means to an end; to show the client that he is not a victim of his stuttering blocks and that he can change and stutter in a different way. As this skill develops the client learns to diminish his struggle behaviors and the stuttering becomes less overtly severe.
Cancellation (Stuttering Modification)
Description: When blocking, the client finishes the word; stops and pauses for a few seconds; then says the word a second time, but fluently. It is important that the client finish the stuttered word rather than stopping when he stutters. Also be sure to pause afterwards so that the muscular tension has time to dissipate. Begin saying the word a second time, but not in a hurried fashion.
Symptom Relief: This technique helps the client recognize and learn how they stutter and how they can change their speaking style to speak with less effort and increase their natural fluency.
Benefits: Cancellations give the client time to analyze his stutter, rest and relax, then say it again fluently. The client should recognize what went wrong when he stuttered and how he should correct it.
Therapy Tip: Be sure the client completes the stuttered word; this reinforces his ability to work through disfluencies rather than yield to them. Pausing is equally important; instruct the client to check that the muscular tension involved in stuttering has completely dissolved. Feeling his speaking mechanism completely relaxed, proceed to say the word again easily and effortlessly.
SUMMARY
Speech targets are tools (or techniques) for a client to master in a series situations of increasingly stress-provoking circumstances. These therapeutic tools may be used on a "as needed" basis in specific situations, or preferably, to change the general manner in which the person who stutters speaks, making it more compatible with fluency. For example, slow rate is a technique that might be used situationally. When giving an oral presentation for example, slow rate benefits not only fluency, but it also makes it easier for an audience to follow and process what is being said. The speaker also sounds and appears relaxed, which often makes him feel relaxed, too.
As a client becomes more capable of managing their stuttering using their targets, their speaking confidence increases while their fears and anxieties decrease; this is a true turning point in their therapy. They now have tools to effect speech fluency. They must also have the discipline to use their new tools.
With the ability to control stuttering and newly learned techniques to enhance fluency, clients become less anxious about speaking. Less anxiety also lessens muscular tension and more natural fluency is forthcoming.
PAGE 35
Counseling and Psychological Aspects of Stuttering
"I don't know if that's what he wanted to ask me, but it's something everybody wants, for someone to see the hurt done to them and set it down like it matters." (from The Secret Life of Bees, p 185, by Sue Monk Kidd)
Counseling in stuttering entails knowing what questions to ask the client, and when to talk and when to listen. Inside every person who stutters is a story; a story of their struggle and their pain resulting from experiencing stuttering. It's the clinician's job to get the story out and make them feel that it matters.
The therapeutic benefit of counseling also comes in the exchange of information between the client and clinician. Each person experiences stuttering uniquely. The client has information about his perceptions, feelings, beliefs, emotions, history, knowledge, and experiences that are vitally important to the clinician to effectively assist the client in finding a successful resolution to his stuttering. The clinician is a resource of knowledge, factual information, and has experience working with a variety of persons who stutter that the client can draw upon to change and progress. Together, the client and clinician work toward constructing a foundation upon which success in therapy is based.
In this section, basic elements of counseling are discussed as they may be applied to stuttering therapy. Another segment provides information about feelings and emotions. This information can be an integral part of counseling.
An Overview
Counseling is the part of stuttering therapy that addresses the client's feelings, attitudes and emotions about stuttering. These personal components are frequently the 'sticking points' or obstacles that inhibit risk-taking, openness to learning, and overcoming habitual patterns of stuttering. They are then, of critical importance to the successful outcome of therapy.
Counseling enables the clinician to learn how the client thinks about issues related to their stuttering, providing avenues by which the clinician may explain or offer alternative perspectives for the client to alter his thoughts and beliefs. Counseling in stuttering therapy may serve several purposes and address issues that include:
OFFERING INFORMATION
- Providing accurate information can clear up misconceptions and enable the client to progress to new levels. Good information can play a significant role in formulating objective, realistic perspectives on stuttering.
- Feelings of embarrassment, guilt, hostility, shame or defensiveness can be spirited into cooperation and sharing.
- Counseling offers a chance to share what is known about stuttering and what is not yet fully understood.
MODIFYING THE ENVIRONMENT
- Teaching the client to perceive environmental stimuli in more objective and productive ways that will decrease negative emotions and enhance fluency.
- Helping the client to find words to acknowledge their stuttering openly and educate listeners about stuttering.
FACILITATING INTERVENTION STRATEGIES
- Providing a philosophical framework upon which therapy is based.
PAGE 36
- Developing independence; helping the client become his own clinician.
- Developing an internal locus of control; empowering the client to become responsible for his or her fluency.
EXPLAINING STUTTERING
Most people who stutter don't know how to explain their stuttering, to themselves or others. The cause of stuttering is not completely understood and is the subject of much speculation and misunderstanding. Some people think it is a sign of an underlying psychological disorder; stuttering is listed under mental disorders in the coding system used by the medical profession. This is truly incorrect. Nonetheless, many people who stutter live under this shadow without any means of disproving it. As a consequence, many who stutter turn these feelings inward and feel badly about themselves, as if something was drastically wrong with them. The following is offered as a way for people who stutter to think about their stuttering and talk about it with others.
Some individuals, about 1% of the population, are born with a predisposition to speak in a different manner; to stutter. This difference appears in men about four times as frequently as it does in women. This is not an intellectual, social or academic difference, but it manifests itself in a breakdown of the fluency of speaking.
Research (utilizing Positive Emission Tomography or PET scan technology) studying how people use their brain when speaking shows us that when people who stutter speak disfluently, they use their brain differently than they do when they speak fluently and differently than people who don't stutter. Interestingly, when people who stutter speak fluently, they use their brain more similarly to fluent speakers.
One of the differences is in the side of the brain that becomes dominant and coordinates the movements of the muscles used in speaking. For 95% of people who don't stutter, the left hemisphere of the brain takes this dominant role in speaking. When a person who stutters speaks fluently, activity predominantly in the left hemisphere is also seen. But when the person who stutters is disfluent, there is nearly equal activity in the left and right hemispheres. In other words, neither hemisphere becomes dominant and consequently, their speech loses its coordination.
A second factor also is prevalent. PET scans reveal that there is considerably more activity in the cerebellum, the part of the brain that coordinates smooth muscle movements. We infer then that when a person stutters, the cerebellum works much harder than fluent speakers trying to coordinate the movements for speech.
When the internal and external demands on the speaking system are too great, the fluency of speech is disrupted. A demand is any situation that causes the individual to exceed their capability to speak in an effortless, coordinated, natural way. Speaking skills are exceeded when the rate of speaking or the effort used to speak increases to a point where it becomes uncoordinated. Disfluencies also result when excess tension in the muscles is used in speaking and producing voice. This tension often stems from anxiety, fear or nervousness related to an individual's reaction to stuttering —embarrassment, shame, humiliation, frustration and the like. Out of fear, many avoid words or avoid speaking situations altogether, which increases their emotional reactions to stuttering and creates greater demands upon the speaking system.
Thus, stuttering is a speech disturbance with two faces - the uncoordinated movements of speaking and the emotional reactions to stuttering itself. Therapy therefore needs to address both aspects of the problem. We use speech therapy and counseling to address a client's many needs.
Clinicians should work with the client to develop their own script; a way of explaining and talking about their stuttering to others when the opportunity arises. It also provides a foundation from which to build a healthy perception of the client's own stuttering.
PAGE 37
MODIFYING PERCEPTIONS AND CHANGING BELIEFS
The clinician should have an end goal in mind to direct their counseling efforts toward; a model to be created in the mind of the patient. There are several approaches or tools available to assist in the counseling process.
An initial step is to learn what the client currently thinks and believes about their stuttering. This is somewhat of a "moving target" in that the client is learning and discovering their attitudes about stuttering even while the clinician is gathering the information. But the process of discussing stuttering can be as important as the information that results. It's therapeutic just to be able to talk about it!
Once the baseline information is gathered, the clinician plans strategies to modify the way the client thinks about their stuttering. At first, the willingness to entertain different thoughts about stuttering is an important step. This flexibility demonstrates a lowering of the client's guard; recall that the emotions of stuttering serve to diminish creative and flexible thinking....this is an initial step toward making change.
TOOLS AND STRATEGIES
Logic. A logical argument is usually ineffective in fighting against emotions. For example, for the patient whose speaking rate is too quick, the clinician might explain that by slowing overall speaking rate, stuttering will be diminished. By stuttering less, the actual time it takes to read a sentence aloud will be reduced by speaking slower. While this makes sense, it will be ineffective in convincing the client to consistently slow his or her rate for more than a minute or two. Rate is governed more by emotions than logic.
Other Feedback Modalities. Getting a "fresh look" at a persistent problem can afford an opportunity to reevaluate beliefs. For example, patients commonly complain that using certain fluency techniques make their speech sound abnormally slow. Having the patient listen to a recording of their speech may change their perception. Some patients, after listening to a recording of their speech, are surprised that it doesn't sound as slow as it seems while they're speaking. Afterwards, they are much more willing to use their targets.
Having a client look at their mouth in a handheld mirror may provide feedback that the client was not aware of. For many, it is rather startling to see that the visual manifestations of stuttering are much more apparent to others than the client believed. This can be a very unsettling discovery, but is often very motivating.
Challenging Beliefs. Some clients have constructed unrealistic beliefs about their stuttering predicament. Challenging these beliefs is one way of dispelling and changing them. For example, many clients are unwilling to talk about their stuttering with others, fearing that their listener will ridicule them. Encouraging the client to test this hypothesis out in a relatively safe environment is one way of facilitating change.
Reframing and Alternate Explanations. It's easy to get locked in a single way to interpret a situation. Clients often lose the ability to see other perspectives on issues. Helping them develop other explanations or reframing situations and events may enable patients to become more flexible thinkers, and change their beliefs.
Confrontations. Sometimes by "looking fear in the face" (confrontation) the client discovers that it is not half as bad as it was built up to be. Being petrified with fear that one might stutter places the client in an "immovable" position. But stuttering on purpose or having a "stuttering contest" (see who can stutter the longest or loudest) can teach the client that fears need not be a part of stuttering.
PAGE 38
COUNSELING OBJECTIVES
Counseling is an important part of stuttering therapy in that it addresses many of the after effects of stuttering and the factors that contribute to its persistence. This is often referred to as baggage. A skilled clinician leads the client through a process of self-discovery to reveal and change many of the underlying feelings, emotions, thoughts, and beliefs about their stuttering. This complement to speech therapy leads to a better resolution to the problem. Some of the objectives of therapeutic counseling are presented below.
- Taking Speaking Risks - Encouraging a client to move outside his or her comfort zone to experiment using speech targets in new and more difficult speaking situations is a key to maximizing progress in therapy.
- Building Awareness, Understanding and Skills to Better Manage Emotions - To be able to overcome the powerful effects of emotions, clients need to examine them more closely, understand how they work, and what they signify to be able to manage them most effectively.
- Revealing the Dirty Little Secret - Most people who stutter try to conceal their stuttering from others. This increases tension and diverts important resources from using speech targets. Finding ways to reveal stuttering to listeners puts the speaker "on top of" their stuttering, rather than facing the burden of having stuttering overpower them.
- Improving Coping Skills - Many clients have not developed skills to effectively cope with their stuttering and emotions much beyond those of childhood. It remains an "area of vulnerability". Learning new ways of coping and processing feelings with adult skills serve to lessen the impact of stuttering behaviors.
- Discovering Other Assets - It's easy to focus on what's wrong and not recognize other personal assets. Taking an inventory from a broader perspective can be a healthy means of putting stuttering in its place.
- Valuing Communication, Not Just Fluency - Many who stutter measure their success communicating with the "fluency yardstick". Realizing that successful communication is not fluency-dependent can become an important foundation for change and acceptance of stuttering.
- Cognitive Restructuring - Developing new vantage points from which to view stuttering can free clients to move to new levels of understanding and "unblock" their ability to change.
- Sharing Troubles - Many adults keep their stuttering problems to themselves. Having someone to listen, understand and evaluate their situation may pave the way to developing a greater openness about stuttering with others.
- Learning about Stuttering - The power of learning factual information, and dispelling myths or misinformation about stuttering, improves coping ability and strengthens the foundation for accepting stuttering.
- Exploring the Emotional History - Helping clients learn why they feel the way they do about their stuttering is an initial step in the healing process. It can provide valuable insights for the clinician in understanding the client's perspective and learning how to help them.
- Understanding Feelings and Emotions about Stuttering - Learning that feelings and emotions reflect underlying beliefs helps demystify them and use emotions to one's advantage, rather than allowing them to control the client.
PAGE 39
TAKING RESPONSIBILITY FOR CHANGE
It seems to be human nature to resist change, especially when that means moving outside your comfort zone. We look to someone else to change for us; anything but doing something differently ourselves. Indeed, many human problems are successfully treated by others; if your child has an ear infection, you take them to the doctor who prescribes an antibiotic and the uncomfortable symptoms of the problem are gone within a few days. But look for a moment at some common everyday problems that seem to defy successful treatment, such as dieting and weight loss. Upwards of 90% of people who have lost weight return to or surpass their previous weight within the first year after their diet. Why? The formula for weight loss is simple — intake fewer calories through eating and expend more calories through exercising. Many however, look to more 'drastic measures' to lose weight: having their stomach stapled, relying on diet pills, or liposuction surgery — anything but taking responsibility to do something differently! Those who are successful at making changes take responsibility. The prognosis for those who don't is poor.
Responsibility for change may be reflected in a client's word choice. For example, acknowledging a stuttering moment as "something happened to me" implies that the client isn't responsible. "I didn't do it, it happened to me." It may sincerely feel that way to the client (which is explained in another section). The client is revealing that he or she feels victimized or out of control during moments of stuttering. As a consequence, the client also feels there is little he or she can do to prevent or even modify their stuttering. This belief is incompatible with a successful outcome in therapy.
The clinician may subtly counter the client's beliefs by asking a question such as "What are you doing when you stutter?" or "Do you feel yourself trying to force air out while you are holding your vocal folds tightly closed?" This wording places responsibility for behaviors with the client/speaker. Being responsible for stuttering also empowers the person who stutters to act in such a way that they don't stutter. Thus, the language of responsibility is also the language of empowerment. This is a primary premise of therapy. "I stutter; I can change. I don't need a pill, I can do it."
In truth, people have misgivings about taking medications anyhow. There is always the potential of serious side effects (such as with Halperdol, sometimes used to treat stuttering). Subjects taking Halperdol reported that the side effects of the drug were worse than stuttering and discontinued taking the medication. But from a broader perspective, many people dislike feeling personally weak or helpless, needing to be reliant upon a pill to effect personal change. While medications may be appropriate, useful, and necessary for treating numerous problems such as heart disease or depression, for the vast majority who stutter, medications have not been developed that successfully change stuttering. Research on promising psychiatric drugs such as Resperdol have demonstrated improvement in as many as 50% of subjects; but 25% of subjects in the study demonstrated a decrease in their stuttering taking a placebo.
Other forms of evading responsibility include hypnosis. Some clients seek the aid of a hypnotist to help them to be more relaxed while speaking and consequently more fluent. Any beneficial effect of post-hypnotic suggestion is usually short-lived, as it does nothing to engage the client's willful participation in being fluent. Most clients experience the phenomenon of being very fluent in the therapy room but very disfluent everywhere else. This usually is a reflection of the client being responsible for their fluency during therapy, but not at other times. As the client accepts responsibility for change, their fluency gradually follows them to other situations. At the beginning of therapy, the clinician assumes the vast majority of the responsibility for implementing fluency targets and making change. As therapy progresses, responsibility is gradually and increasingly transferred to the client to effect changes in their speaking patterns. Gaining a sense of being able to effect change in one's stuttering is very empowering and a fundamental experience toward managing fluency.
PAGE 40
WORKING WITH ANXIETIES AND FEARS
Anxiety and fears about speaking are common among people who stutter. Fear is a very primitive bodily response to danger; it is fundamental to sustaining life. People need to be cautious and avoid serious dangers. Anxiety is related to fear; it is a general feeling of apprehension; a premonition of danger nearby. An intense, excessive fear of an activity, object, or situation is known as a phobia. With phobias, the fear is out of proportion to the actual physical danger at hand. A phobia causes a person to make alterations to their life in order to avoid perceived physical or psychological dangers.
The Role of Anxiety and Fear in Stuttering. Anxiety, fear and phobias are commonly an integral part of the problem of stuttering. Speaking phobias result in limiting or restricting activities in which patients are willing to participate. As a consequence, these avoidances and restrictions handicap their lives.
For those who stutter, patterned behaviors, negative thinking, and a belief system emerge that magnify the intensity of the problem. These thoughts and behaviors become internalized and the person who stutters begins to organize their life around their fears about speaking. They begin to form their self-concept around the inability to speak.
Fear and anxiety can represent a bigger problem than the stuttering itself. The thought patterns and belief system contribute heavily to relapse. The body's response to fear and anxiety blocks access to therapy targets, particularly during moments of stress. As a result, many who stutter stop speaking, rather than risk stuttering.
The Body's Response to Fear: There are three components of fear: behavioral, cognitive, and physiological. Behavioral symptoms include such things as shakiness, throat clearing, and avoidances. Cognitive symptoms involve difficulty thinking, hypersensitive or selective stimulus focus. Physiological symptoms include increased heart and respiration rates, and increased blood flow to large muscle groups.
How the Response is Elicited: The emotion of fear is elicited when an event or situation is perceived to be threatening. The person becomes aware on the impending danger — a threat to the ego or the person's sense of self.
Two factors enhance the fear response: past experiences and apprehension. Previous negative experiences in similar situations are stored vividly in memory. These emotional memories serve to accentuate the memory of the event or situation. Apprehension makes the bodily systems that scan for danger more sensitive; it sets them "on edge". Apprehension heightens the impact of fear.
A Deeper Understanding: The body's response to fear is a "call to action"; the "fight or flight response is instantly summoned into play. This primitive reflexive response, however, is detrimental to speaking situations. Both fighting and fleeing involve activation of large muscle groups, rapid heart rate and respiration. Mediation ability through higher cerebral thinking is minimal. These bodily reactions are exactly the opposite of what is needed to effectively manage fluency. The "fight or flight" response is rooted very deeply in our genetics and will not be extinguished. Therapy then becomes a matter of learning to mediate these reactions.
Treatment of Fears and Anxiety: The overall treatment paradigm to manage the fear response is to combat it mentally. Remember, it is unrealistic to expect the reflex to go away; it is primitive and still critical to our survival. One approach is to begin to make fear more tangible and objective. Our approach will be to become more knowledgeable of the fear.
Increasing Cognitive Awareness: It is human nature to want to avoid fears. But to overcome them, one must become more knowledgeable about them — knowledgeable of both the bodily feelings and the object of the fears.
PAGE 41
There are three areas in which patients should learn more about their fears: (1) how their body specifically responds to fear, (2) being able to evaluate the intensity of their fear response, and (3) building more tolerance to the fear response.
(1) Clinicians should explore with patients the ways their body is specifically affected by fear. The "Body's Response to Fear" can serve as a framework to guide the client's exploration. The more detailed the exploration, the richer and more complete the understanding. This knowledge can be used to add rationality to the sensation of fear.
(2) Fear is based upon perception, and as such, can be measured on a perceptual scale. Have the patient assess the level of their fear relative to the extremes of the scale. Commonly, they are asked to rate their fear on a 10-point scale, with 10 signifying an immediate, unstoppable, life-threatening event and 1 being a state near sleep. The scale helps the patient cognitively evaluate, critically compare and communicate the status of their mental and bodily response to fear. Instead of fleeing, they are using their intellect to analyze and grade their fear response.
(3) The point is not to make the fear go away, but to be able to tolerate it better, so that the fear reflex is not set off. This may be approached by listening to the instructions you give to yourself in fearful situations. These instructions may not be words, but rather "impulses". The first step then is to interpret the impulses by "translating them" into words. Being able to articulate the messages is an important initial step toward modifying and changing the message, to allow the patient to respond differently.
FEELINGS AND EMOTIONS: THE EMOTIONAL REFLEX
Many who stutter experience the feeling of being out of control when they stutter. At the moment of stuttering there is a diminished sense of awareness; not knowing and not being able to explain what happened. This "cognitive blackout" is coincident with the stuttering block and might be explained as an "emotional hijacking" or emotional reflex.
The concept of "emotional reflex" stems from the physiological studies of LeDoux. Its psychological application is credited to the work of Daniel Goleman in his book Emotional Intelligence.
You will notice that many clients sincerely attempt to use their speech targets in anticipation of a stuttering event. However, as the moment draws to bear, they are unable to summon their target and they stutter. They are unable to explain what happened. Their best effort to explain their inability to use the target is generally "I forgot" or "It didn't work" - aware that they didn't use the target they planned to use, but totally unaware of what happened in that one split second. They lose control and conscious awareness of a critical aspect of the event.
Briefly and simply, LeDoux found neural interconnections between parts of the brain which "shortcut" the process which triggers the body's response to "emergency alarms". This shortcut bypasses the higher cortical functions (our intellect) which enable us to use the reasoning process to determine the precise nature of the alarm and how we should appropriately respond to it. For example, you hear a mysterious noise in a room in your home; you go to investigate. As you walk into a room your five-year old jumps out from behind the door and says "BOO". In that moment your body instantly and automatically responds in total "terror" as if you are about to be slain. You have just experienced an emotional hijacking. In the next second or two, after your intellect has a chance to process the event. You are able to determine your life is not threatened; it is only a "joke". In that instant you are unable to explain why your shoulders raised and your head "ducked"; you did not volitionally move your body parts, it was a reflex.
PAGE 42
Anticipation of an "emotional event", particularly an event involving fear, serves to heighten the response. This was the hallmark of the work of the film producer Alfred Hitchcock. The fact that the audience knew what was going to happen and was made to agonize, squirming in their seats waiting for the event to take place, was part of the genius of the filmmaker. For the person fearfully anticipating stuttering, the emotional component of the event is similarly heightened.
Likewise, people who stutter are emotionally hijacked at the moment of stuttering, overwhelmed by emotion, unable to intellectually process the event. Their cognitive awareness diminished in the moment of stuttering. Emotions heightened by the anticipation and fear of an upcoming stuttering event.
ASSESSING KNOWLEDGE OF STUTTERING
Learning to cope with stuttering is an important goal of therapy. Coping includes becoming better adjusted to stuttering, being able to view it objectively and accepting it as part of the person you are. This process of coping is based upon developing accurate information and building personal beliefs about it. This is not an easy task; it is usually a lengthy process. Stuttering is poorly understood by the public; even by most speech-language pathologists. There is a great deal of misinformation about it. This often results in the patient suffering needless anguish that interferes with their ability to cope with their stuttering. It is therefore important that the patient develop a knowledge base of their stuttering. It is the clinician's role to assess the client's current knowledge and understanding of stuttering, and provide more accurate information as necessary. From a solid information base, the patient can begin to define their stuttering, and begin the process of coping and accommodating it.
In evaluating a client's knowledge and understanding of their problem, there are a few areas that may be fruitful to investigate. The clinician might discuss these following topics with the client, evaluating their responses for accuracy and objectivity.
Some clients are only able to offer minimal information about their stuttering. It may be difficult to talk about or they may lack awareness of many features of their stuttering because the experience is very emotionally negative.
Responses to these and other inquiries reveal the client's awareness, objectivity, and perceptions of their difficulties. These questions may open a dialogue about stuttering that the clinician can begin to inform, challenge, and develop rational beliefs about their difficulty.
This will be an ongoing process in therapy; one which takes time. When the clinician has developed their own belief and philosophy about stuttering, the job of directing the client and shaping their beliefs becomes easier. It is not uncommon that just talking about stuttering becomes therapy itself; for many, it is a very emotional part.
CONCLUSION
At best, the fears and anxieties associated with stuttering can be better managed; it is not reasonable to think they can be extinguished. It is difficulty for many people who stutter to comprehend that people who don't stutter are the least bit anxious or fearful of public speaking. Learning how to mediate the process by which fear and anxiety is elicited and communicated throughout the body can be an effective means of managing the response, enabling the client to function appropriately.
TYPES OF CLINICIAN RESPONSES
Effective counseling is most often client-centered. The counselor (clinician) waits to hear the issues the client brings to the table before responding. Counselors begin where their client currently is and directs them ahead from there.
The following types of interactions are brief examples of responses a clinician may use in responding to a client in a counseling session:
PAGE 43
Affirmations: Being a positive sounding board for the client. "Having the power and wisdom to say nothing."
Content Response: Information is communicated which is factual, straightforward and brief.
Counter Question: People often don't want advice, but seek confirmation of their position or decision. Clients often don't learn from advice and it doesn't promote their decision-making ability. Questioning a client's expressed beliefs is a means of helping them question themselves. Counter questioning moves the relationship beyond an initial or information exchange stage.
Affect Response: Try to see the world as the client does and reflect their feelings back to them. Inaccurate reflection forces the client to clarify their position and your understanding.
Reframing: Finding an alternate perspective that makes an event seem somehow more acceptable. Good reframing should give the client a "jolt".
Sharing Self: Sharing your personal insights and experiences enable the client to view you as human and imperfect, just as they view themselves; this usually results in enhancing the relationship.
Silence: A technique that encourages the client to talk more; the implied expectation that the client is to continue talking.
- Embarrassed Silence: In the initial stages of the relationship, establishes power; diminishes familiarity.
- Changing the Topic Silence: While each party reflects on whether they have more to say on the current topic.
- Reflective Silence: Follows an emotionally laden talk; taking a timeout to think.
- Termination Silence: As time grows close to the end of the session.
Skillful use of these responses takes time and practice to master. Keep in mind, the goal is to find productive ways to facilitate the client's willingness to contribute to their own care.
PAGE 44
Evaluating Stuttering
A stuttering evaluation consists of a review of the client's history relevant to their stuttering, a description of the current status of their stuttering, a cursory assessment of other communicative abilities (voice, articulation, language, and hearing) (more in depth if they contribute to stuttering), evaluation of the functioning of the oral peripheral mechanism, and a summary of the findings. Minimally, the purpose of the initial evaluation is to gather basic demographic information, establish a diagnosis, document baseline disfluency data, assess factors contributing to the stuttering, explore therapy techniques, and agree upon a future course of action.
The information offered below details these segments of an evaluation.
A thorough assessment of stuttering is a process that happens over the course of time. Most of the truly important information does not emerge until the relationship between the client and clinician has a chance to develop. There is however, a minimal set of elements that do need to emanate from the initial interaction. They include:
- gathering basic demographic/contact information
- establishing a diagnosis
- documenting baseline disfluency data (severity rating and description)
- assessing factors contributing to the stuttering
- exploring therapy techniques
- agreeing upon a course of future action
Many factors do not emerge until later as the client may not be:
- ready to reveal emotionally-based information at the outset
- knowledgeable of the importance of some factors
- aware of variables that relate to his or her stuttering
There are not always formal tests to evaluate some important parameters of the client's stuttering. Further, a client's beliefs and perceptions (rather than structural or developmental abilities) strongly influence their behaviors and performance. Revealing these beliefs and perceptions takes time and trust, and many clients are often not ready to discuss them in the initial session.
Clients usually seek an evaluation because they are not able to resolve their difficulties on their own. There is often a sense of helplessness and frustration that accompany people in this situation. The clinician is a ray of hope and must act judiciously, walking a fine line between instilling hope and conveying a realistic picture of the hardships that lie ahead in therapy.
There are several components of an evaluation; each are presented in more detail. They include:
| Background Information | A history of the development of the client's stuttering, past therapies, family history of stuttering, the outcome they expect from the assessment, how stuttering affects their life |
| Communication Abilities | A report of their skills in the five parameters of communication - stuttering, articulation, voice, language and hearing ; oral motor function |
| Prognosis | A review of factors which are likely to promote and hinder the successful outcome in therapy |
PAGE 45
BACKGROUND INFORMATION
The objectives of the background section of the assessment are to:
- Trace facets of the history and development of the stuttering
- Determine what has been done to change the stuttering (past therapies, techniques, etc.)
- Find out how the client perceives his or her stuttering
- Learn how stuttering affects the client
- Learn the reason the client has sought to do something about his stuttering at this time and the expected outcome of today's session
- Determine the client's understanding and objectivity toward their stuttering
This information is gathered in an interview in which the clinician asks questions and probes the client with the goal of ascertaining specific facts involved in their stuttering. The following list of questions should be considered as a framework from which to probe clients to elicit the desired information. Remember that every client is different and each interaction with any given client will differ. It is up to the clinician to interact with and lead the client's responses in order to garner the necessary facts and the client's perceptions.
Typical questions might include the following:
- What brings you here today? (How are you looking for us to assist you?)
- When did your stuttering begin? (At what age did it start?)
- How has it changed since it began? (Determine the course of stuttering development)
- Does anyone else in your family stutter? (Is there a family history of stuttering?) Do they still stutter, or did they recover? (A prognostic indicator)
- Have you ever gotten help for your stuttering before? (What's been tried; how successful was it; why didn't it continue to work?)
- What physically happens when you stutter? (How well can the client objectively describe the parameters of their stuttering?)
- Are there particular sounds, words, or situations that you find difficult? (Are there feared factors or situations that the client has learned?)
- What do you do to help yourself in these situations? (Can the client do something that is helpful or do they find themselves a victim of their stuttering?)
- What do you think causes your stuttering? (Determine what the client knows — or thinks they know — about stuttering)
Note the stuttering behaviors the client exhibits in responding to your questions. The background information usually takes about 10-15 minutes to gather in the initial segment of the assessment. Remember that the client has told you how to "satisfy" them at this initial meeting (what they are looking for). Be sure to orient your summary of the evaluation at the end of the session toward answering the client's specific reason for coming, even if that's not the most "professionally" significant assessment finding.
PAGE 46
COMMUNICATION ABILITIES
Stuttering
The stuttering section describes the attributes of the client's stuttering behaviors, rates severity, describes maladaptive speaking behaviors and probes stuttering's handicapping affects on the client. Assessment of each component is described below:
- Stuttering Behaviors: Enumerate all core stuttering behaviors (blocks, repetitions, prolongations, and tremors) observed during the session; provide an approximate prevalence of each behavior noted.
- Secondary Characteristics: Describe all bodily movements, interjected sounds, avoidance and escape behaviors, and "non-speech" components associated with stuttering.
- Severity of Stuttering: Using the Riley Stuttering Severity Instrument (SSI), determine the severity of the client's stuttering. There are three components to the SSI — a frequency count of the client's disfluencies in spontaneous speech and in reading, the duration of their three longest disfluencies, and a rating of distractibility of secondary behaviors. [Note: The SSI-3 tallies disfluencies at the word, rather than the syllable level. While looking at syllables may be more sensitive to changes in stuttering, the additional time required to analyze the speech sample may not be justified, particularly in light of other variables unaddressed by either version of the assessment tool.] Video record a 150-word spontaneous speech sample; try to elicit the sample without needing to interrupt or question the client in order to have them speak 150 words. Next, have the client read a 150-word passage, taking care to select a passage that will not challenge the client's reading ability. A video is available on the SLP Blackboard site that provides more detailed information on administering the SSI.
- Maladaptive Behaviors: Note any unusual or effortful speaking behaviors evidenced during the speaking and reading samples and previous conversation. Such behaviors may include rapid rate of speaking, excessive muscular tension in the lips, tongue, or throat when articulating sounds, hard glottal attacks, loss of eye contact, pauses and hesitations, interjection of extraneous sounds or phrases ("you know", "like"). While not an exhaustive list of possible behaviors, these are the most common.
- Handicapping Effects: Discussion of how the client copes with his stuttering may be elicited by asking questions such as, "How do you think your life would be different if you didn't stutter?" The clinician seeks to determine the accommodations the client makes because of their stuttering. A handicap is defined as what the client does or does not do solely based on their stuttering.
Clients are asked to try a variety of speech therapy techniques, based upon the symptoms of stuttering they exhibit or the philosophical orientation of the clinician. This experimentation serves to determine a likely starting point for therapy. Determine the client's most frequent stuttering behavior and select a fluency target that enables them to change or compensate for the dysfunctional aspects of their disfluency (see the section on fluency techniques).
Note the techniques the client used successfully and did not express reservation using. For some clients, this will be their first experience in being able to exert any degree of control over their stuttering. This can be very exciting and the foundation of hope for their future. Clients often express reluctance to use slow rate as a technique outside of the therapy room. It is sometimes unwise to attempt to convince them of the virtues of speaking at a slow rate during the initial session; generally clients discover it on their own at a later point in their therapy.
PAGE 47
Articulation
Children who stutter have a much greater likelihood of having an articulation or language problem concomitant with stuttering. An experienced clinician will note the presence of misarticulated sounds in the client's conversational speech. If none is noted, there is no need to administer a formal articulation test. The clinician simply notes that "No significant misarticulations were noted in the client's conversational speech."
If some sounds are misarticulated, a formal articulation test is administered to inventory errant sounds. If English is not the client's native language, vowel production should also be assessed. The Goldman-Fristoe Test of Articulation or the Arizona Test of Articulation are common choices. Because articulation tests are commonly developed for children, their stimulus pictures are also age appropriate for children. A brief explanation to clients about the drawing's simplicity is usually sufficient to avoid 'offending' adult and adolescent clients.
Many people who stutter have difficulty with confrontational naming tasks such as those required in articulation testing. The purpose is to evaluate production of a specific sound, not to retrieve the name of the stimulus word. With that in mind, the client may be allowed to substitute another word with the sound in the same position. Note the sounds that seem to elicit stuttering responses; you may later determine that certain sound production categories (such as plosives) tended to be stuttered on with more regularity by the client. Remember, with adults, age norms are not meaningful — they should already have mastered all phonemes.
Some stuttering clients have "slushy" or "sloppy" articulation skills. The articulation of specific sounds may not be "bad", but the overall quality of the ability to precisely move the articulators is poor. For these clients, their oral motor abilities may be suspect and may contribute to their stuttering. A client's articulation ability is generally a good indicator of the functional ability of their oral peripheral structures.
Voice
Clinicians must also be cognizant of the parameters of normal voice production: pitch, intensity, quality, nasality and resonance. When noted in clients who stutter, voice disorders are most often unrelated to their stuttering. There are however, several parameters related to voice that are commonly seen in people who stutter. They are described below:
- Ineffective Breathstream Management: Rapid inhalation of air or gasping, or speaking on residual air
- Abrupt Vocal Onset: Beginning phonation abruptly rather than softly and smoothly; typically with excessive force
- Hard Glottal Attack: Phonation begins with the vocal folds forcibly held together; usually there is a failure to release any exhaled air before adducting the vocal folds to initiate phonation
- Pitch Rise: As a block continues, the client's pitch fluctuates (usually rises) as they attempt to force their way through a block
- Loud Voice: Usually the byproduct of effortful speaking attempts
- Soft Voice: May reflect fear or lack of confidence in speaking
Many of the therapy techniques for stuttering specifically address these voicing parameters. Consequently it is important to be familiar with them.
PAGE 48
Language
The clinician gets a general sense of a client's communication skills by how well they are able to put their thoughts into words and follow a conversation. Clients demonstrating functional abilities to express themselves and understand what is said to them usually do not require further language testing. Assessment of language skills in adults (who have not suffered a stroke or other neurological insult) is generally a matter of some subtlety. It is thought that language impairments are present among adults who stutter no more than the general population. (However, it has been reported that 24% of children who stutter have concomitant speech and/or language problems.) Certainly word-finding difficulties may distract from the overall fluency of a client's speech. However, many clients who stutter substitute another word for one they think they will have difficulty saying. As a result, their communication may sound awkward or is frequently revised to accommodate their avoidance strategy. Additionally, many people aren't willing participants in conversation and don't provide much opportunity to informally assess their language abilities.
The dilemma then is 'what to test'?
- Vocabulary Development: The Peabody Picture Vocabulary Test (while dated) does not require a verbal response and also provides estimated IQ information, which for some clients, may have prognostic value.
- Word Finding: The Naming subtest (Section IV, B Word Fluency) of the Western Aphasia Battery may provide a rough indication of the client's convergent word-finding abilities. Responses can be written instead of spoken.
- Sentence Formulation and Syntactic Development: Elicited in a writing sample; have the client write a brief essay or describe a picture.
Clients who present with a neurogenic incident in their history may require more testing specific to areas of possible language and cognitive impairment. Stuttering evidenced subsequent to neurological trauma is substantially different than developmental stuttering in its symptoms and treatment.
Hearing
Hearing ability is best evaluated using an audiometer and a sound booth. Impaired hearing acuity is not commonly related to stuttering, so functional measurement is sometimes adequate for purposes of the fluency evaluation. The clinician may get hints of hearing impairment by a client's frequent requests for information to be repeated or their misunderstandings in conversation.
To administer a functional hearing test, the clinician conceals of their mouth from the client's view with a paper or other object. The client is asked to repeat numbers or letters presented by the clinician in a whispered voice. The clinician includes a "trick" word in the series of number or letter presentations? "Six three nine... seven... elephant". By using an item outside the expected 'data set', the client's ability to use guessing as a means of responding is frustrated.
People who stutter do not evidence hearing loss with greater frequency than the general population. However, some research tends to indicate that the auditory processing ability of people who stutter differs significantly from people who do not stutter.
PAGE 49
Note: Periodic hearing testing is an important part of responsible hearing care. Many people suffer from chronic middle ear infections, have a history of exposure to noise or have difficulty understanding others in noisy environments. Referral for an auditory assessment may help remediate these difficulties for clients.
Oral-Peripheral Examination
Structural abnormalities are not commonly associated with stuttering and therefore are no more likely to be found among people who stutter than the general population.
A client's articulation ability is generally a good indicator of the functional ability of their oral peripheral structures. In particular, listen for the 'crispness' of sound production and for inconsistent articulatory placements as indicators of potential decrements of function. The client's stuttering often impairs the clinician's ability to assess functional movements in speech. Some who stutter use excessive effort in articulating sounds associated with stuttering.
Rate of speaking may be another issue. When assessing rate, consider that each individual has an optimal speed at which the articulators function accurately. The clinician can judge whether the client's habitual speaking rate exceeds their optimal articulating speed.
Another measure of oral mechanism function is diadochokinetic rate. For many clients who stutter, stuttering impedes diadochokinetic testing for reasons similar to that of confrontational naming tasks. If the client has difficulty with "pataka", try "buttercup" or another multi-syllabic words. Actually counting syllable rate production is less important than gleaning a feeling of the synchrony and coordination of the mechanism. In my experience, there is little 'middle ground'. Either the client does well, or they don't.
Introduce each sound individually; have them repeat "pa" as rapidly as they can for at least 20 seconds. Do the same for "ta" and then "ka". Note their ability to maintain continuity of movement at rapid rate. Be mindful of disfluencies. Next, ask the client to repeat the entire sequence, "pataka", as rapidly as they can for at least 20 seconds. Again, the exact rate is less important than the integrity of movement.
"Slushy" articulation, drooling, problems with saliva control or 'messy' oral habits (such as eating) at present or in the client's past, brings delayed or disordered oral motor function under suspicion.
SUMMARY INTERVIEW
At the conclusion of the evaluation the clinician has the opportunity to communicate important information to the client. Recall that the minimal components of the initial evaluation are to gather basic demographic information, establish a diagnosis, document baseline disfluency data and agree upon a future course of action. This then represents an outline about what will be communicated.
The demographic information is usually obtained on the Clinic registration form. In a brief time, the clinician usually is able to establish the diagnosis of stuttering (primarily for insurance purposes). During the summary interview, the clinician reviews the components of the client's stuttering that were observed during the assessment, along with an explanation/description of each. Additional information about the course of stuttering's development, cause, or other pertinent information is also communicated. It is critically important to respond directly to the purpose the client initially expressed as their reason for seeking the evaluation. This provides a sense of satisfaction for the client and often is the beginning of a new set of questions yet to be addressed. The final feature of the evaluation is to recommend a course of action for the future. The client is
PAGE 50
entitled to the clinician's best advice and direction in resolving the problem(s) presented during the assessment. After making recommendation(s), the clinician discusses the options and assists the client in making a decision about a course of action to pursue, but the client decides what to do.
The evaluation report is another opportunity for the clinician to communicate the results of the assessment. Usually there is too much information to successfully communicate orally to the client. The written report presents all assessment findings, interpretations, and recommendations. As a consequence, the clinician may highlight the most critical findings and recommendations after the conclusion of the diagnostic session, rather than attempting to give a comprehensive report of the assessment in person. The written report also is the clinician's legal document of their findings and a tool used to communicate with other professionals.

